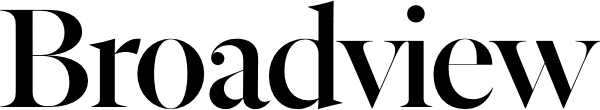
Following a March reader survey on life and death ethical decisions, The Observer invited representatives from the Winnipeg faith community to discuss religious responses to the emergence of clinical euthanasia and physician-assisted suicide as major legal and social issues.
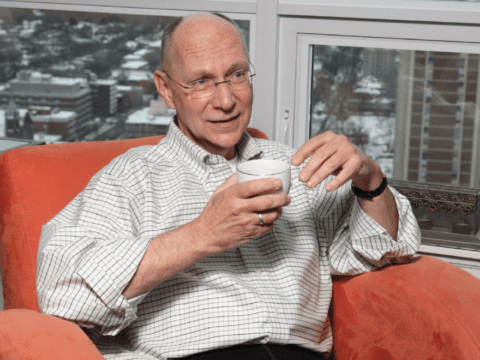
The conversation, held at the University of Winnipeg, included the following participants, in alphabetical order:
- Rev. James Christie (professor of theology, United Church)
- Pundit Venkat Machiraju (Hindu Society of Manitoba)
- Marion Magnusson (neonatal chaplain, Anglican)
- Dr. Redwan Moqbel (professor of medicine, Baha’i)
- Rabbi Lawrence Pinsker (Shaarey Zedek Synagogue)
- James Read (ethicist, Salvation Army)
- Sensei Fredrich Ulrich (Manitoba Buddhist Temple)
- Prof. Ludmila Zamah (lecturer in religion and culture, Muslim)
Observer editor David Wilson moderated the roundtable discussion. The transcript below has been condensed and edited for clarity.
Observer: Speaking as individuals, would you want the right to end your life with the help of a loved one or a doctor? Would you want a doctor to take measures to end your life if you were unable to do so yourself?
Fredrich Ulrich: In Buddhism, one of the taboos is for a priest to counsel suicide. So that puts me in a bind about myself. But I think that I would say yes. But it needs to be collaborative, involving me and my family, not just the doctors.
Venkat Machiraju: In Hinduism, we believe that when the soul’s turn is over, it has to go. If you terminate suffering, you have to undergo it in some other place or in some other life. So we have to let the suffering go on, though we can take measures to reduce it. We cannot forceably end life, but rather let it phase out by itself. If you take a person off a life-support system and the person can go freely, I think that should be an option.
James Read: I’ve been around enough people in agony to think that yes, I could be there. I hope, I pray, that I never am, but I can see it. But it’s a different matter from whether I should have a moral or legal right to do it. I think there is a pretty deep-seated sense that we receive our life as kind of a trust, so when we take into account what it is we would want, that would certainly be a material factor.
Lawrence Pinsker: I wonder whether the questions boil down to two variations on the same theme. The first being, what informs the decision to terminate a life, whether I choose to do it or someone else chooses on my behalf, if I’m unable to? Faith is one instrument whereby one can make a decision of that nature, but it may not mean the same to Hinduism, Islam, Judaism, Jainism, Buddhism and so on. The second is, whose knowledge base, and whose set of guidelines, is fit for the task of saying this life is no longer able to be sustained?
We assume that quality of life must be an absolute bottom line. But there are people who are prepared to suffer for the sake of an objective, and I’m speaking from personal experience with a person who was stricken with paralysis from the eyes down. When offered the option of termination with physician assistance, this person waffled, astonishingly, and then chose life and lived many years — to see grandchildren born, to see them learn to read, and to be able to communicate with blinks.
I cannot conceive of doctors making a decision on these matters in a manner that would be consistent with faith or an ethical system, because I don’t want to define only by faith the criteria that move us to make such a decision. So I think the issues are much more complex and need to be unpacked very carefully.
Redwan Moqbel: For me, there are two separate issues here. The first one is principle, or principles, because faith deals with principles. And the second part is the pragmatic application of these principles. My understanding from reading about most religions is that God is the creator of all of us, and as such has given us a spiritual capacity to live life, to enjoy life and to suffer in life also. And that every single aspect of this has a place.
I’m somebody who actually went through this. In 2006, I had the most aggressive form of cancer you could imagine, sinus cancer that was eating my skull. The headache was 24/7, truly unbearable. Not for a second did I entertain the thought that I wanted to end this. No, I actually went back to the principles: what is the purpose of pain and suffering? For me, it becomes very clear that pain and suffering are the same as the friction needed to turn a piece of carbon into a diamond. It is there to refine us. It is there to strengthen us.
I’m still talking principles. But if it comes to the actual decision about ending life by choice, I think the decision needs to be left to the individual based on consultation with skilled physicians. And with the family.
Observer: Has anybody ever had to make a decision for a parent or someone who was unable to make the decision?
Lawrence Pinsker: I actually have to be very careful, because this person whom I mentioned earlier was a person of some celebrity. Suddenly, in the midst of a tennis game, this intelligent, gifted human being just fell, unconscious. When he was brought back to consciousness, he had no mobility. In that situation, there were no guidelines. The doctors assumed that the best thing to do would be to not permit him to suffer. But they wanted some assurance. And we devised a system of communicating involving blinks of the eye. To validate that his blinking was a system of communication was in and of itself something extraordinary to achieve.
I was put in the position of having to make the decision. The doctors handed it to me. To my astonishment, his wife and son handed it to me. Ultimately, he decided to live. And what took his life after almost a decade were the complications of being bedridden and immobile constantly.
Fredrich Ulrich: I come from a community that’s still based largely on the extended family. In a situation I was involved in, they were going to disconnect the grandmother [from life-support]. They invited me in, and we all got in a circle and did a loving-kindness meditation together, holding hands. Then they asked me to leave. It was a collaborative family decision. I think that’s the major thing; it has to be collaborative. But now we’re in a situation where a lot of people don’t live in extended families anymore. Sometimes it’s just me and one or two other people and the person involved. That’s a different problem.
James Christie: I’ve become increasingly aware of the terrible burden of nuance. And the first issue to me is terminology. I think it’s necessary to be very candid that the language we use is the blunt, harsh, real language that says we’re taking a life. That precludes our capacity to soft-pedal. The awesomeness of the decision needs to be very present.
In one case of the ending of a life of a person very dear to me, it was quite clear that not only was the pain unbearable, but the body of this very elderly person had become a prison, and was being acknowledged as a prison by the person. The way to achieve an end in this case was relatively passive: regular injections of hydromorphone were provided by the medical staff in such a way as to gradually suppress the person’s capacity to breathe. So they drifted away quietly and peacefully.
Coming back to how we ourselves might consider our own deaths. . . . Having been personally close to death on one occasion, the idea of death in and of itself long ago lost its terror. But the idea that I might not be aware of leaving this life still fills me with a great deal of anguish. It seems to me that death is our last task. And I want to be able to face that task. So there’s another area of nuance.
I appreciate the comments around the question of collaboration, and yet I’m torn. Though our lives may not be, in a sense, our own, but rather God’s, we are still granted the great and terrible privilege of being independent actors. And in the final analysis, if I am to find that my life needs to be hurried along toward its end, I would hate, as an individual, to pass the burden of responsibility — that terrible burden of nuance — on to someone else.
Marion Magnusson: I want to make a comment about how cautious we have to be about language. The [Observer’s] survey speaks of euthanasia, and then speaks about a physician ending the life of a terminally ill patient by withdrawing treatment. That is a conflict in language. It is not in fact euthanasia for a physician to withdraw treatment. It is done in a collaborative manner, with all of the physicians, caregivers, family and the patient present. A week ago, I was present in a family meeting for an infant that had been on life-support, incubated and living precariously for almost a full month. There was brain damage. So it came down to the parents making the decision. As a chaplain, my position was to help them understand that they were not assisting in the child’s death. They were in fact assisting in easing the child’s pain.
This is where the language has to be really clear. I think this is something that we too quickly say is euthanasia. It’s not withdrawal of the treatment that ends a life; it’s the fatal pathology of the disease.
Observer: The Supreme Court of Canada has agreed to hear a case involving a 60-year-old Muslim man who has been in a coma for two years. The man’s wife insists that he is mentally alive but trapped in a paralyzed body. His doctors want the court to clarify who has the final authority to make decisions on whether people in conditions like this live or die. This will be a significant ruling. To what extent are these questions already on the radar of your faith communities?
Ludmila Zamah: I think these issues are becoming very important to faith communities. We’re in a pioneer phase right now. In Islam, there’s a huge disconnect between the scholars who are making pronouncements and the doctors who have the medical knowledge. And what happens is the authority tends to lie in the hands of the physicians. The theologians don’t have the training to deal with all of the medical nuances.
But there are academics writing about these issues in medical journals. In medical training nowadays, nurse practitioners, nurses and doctors are getting some sort of religious course. I think we have to give them a little bit of credit. They’re not always saying, “These faith people, how irrational they are.”
In classical Islam, the soul is in the heart. When the heart stops, life stops. But the wife in the [Supreme Court] case feels that her husband’s mind is still alive. That’s showing her perspective that the soul is in the mind. So there’s evolution of thought within the religious tradition.
Lawrence Pinsker: I was sadly involved in the famous case here in Winnipeg of Mr. Golubchuk, which generated a court case and the intervention of the physicians’ college. The physician who finally broke through the ice jam that was obstructing a functional decision did so on ancient Jewish philosophical and religious principles: there is a point at which you say this person is dying, and you may not do anything to hasten death, nor may you do anything to retard death. People want some guidelines, but I think it’s an abstraction until the moment they’re in the room with their mother, father, sibling, child. And in that moment, “What do I do?” becomes “Give me solutions. Don’t give me arguments.” They do not want collaboration to mean “It’s up to you.” They’re actually looking for higher authority in some form.
James Christie: We ought to deal with the question of abstraction with the utmost seriousness. It’s at a level of abstraction that laws are made. And one of the things that concerns me is that law is often generated by a sense of expediency. Where faith traditions can excel is dealing with the issue of nuance in individual circumstances. But we’re not, generally speaking, being brought into the conversation on a public policy level. In fact, given the increasing polarization in Canadian society that Reg Bibby describes in his recent book Beyond the Gods and Back, we’re liable to find ourselves increasingly shut out.
Fredrich Ulrich: I’d like to mention the abstraction of religious practice. And one of the practices in Buddhism is letting go. I’ve seen this happen with the elderly; they decide it’s time to go, and they simply let go. There’s nothing evil happening. Are people who practise this committing suicide? Are others who practise it with them assisting a suicide?
James Read: This issue comes up more and more because it’s not me deciding when it’s my time to let go; it’s me deciding when it’s Mom’s time to let go — when Mom can’t speak for herself. I think that deciding for other people has a lot of us agonized.
Fredrich Ulrich: Sometimes, even depriving a person of death is an ethical issue. Death is part of the living experience that we all share. I don’t know what the legal dimensions are, but you sometimes have a sense that you can’t rob a person of their death, because that’s robbing them of a spiritual experience.
James Christie: I want to emphasize the observation Ludmila made about us being in a pioneer phase. One of the things that strikes me is that this conversation could not have been held a generation ago, possibly not even 10 years ago. There is a simple reality of the number of faith traditions that are gathered around the table to begin with. The second reality is the almost inconceivable advances that have been made in medical technology: it’s sometimes difficult to know when the treatment may be more harmful than the actual disease. But it’s also a brand new experience in terms of cultural mores. When I was a boy, suicides were not buried in hallowed ground. And that was not simply the Roman Catholic tradition. Suicide was considered a crime against God and against society.
No one had begun to consider that there might be a variety of understandings around the end of life. We’re now finding in Canadian society the most extraordinary laboratory of faith and philosophical positions that may exist on the planet. So this is pioneering for religion, for medicine, for law, for legislation, and it’s certainly pioneering for individuals and families.
Lawrence Pinsker: I’m wondering whether you’re pushing us toward a boundary issue — the definition of a person. It is not taken for granted in the culture today that there is such a thing as a soul. The distinctions made in classical Judaism, for example, between soul, life force and spirit are irrelevant in a scientific world in which human beings are viewed as biomechanical entities, which terminate the way a machine fails or a library card expires.
James Christie: Gives a new meaning to punching your card!
Lawrence Pinsker: Religion says there has to be some other set of criteria for evaluating life. Otherwise it becomes a marketplace.
Observer: Is there is a danger that our market-conscious culture is going to deal with abstraction by focusing on economics?
Lawrence Pinsker: If there is an elephant hanging over the table, that is it. How much can I afford to spend on one person if the same money will provide health care and preventative medicine for 100,000 people? Do I value the one over the many, or the many over the one? It’s the cultural crisis of every civilization, every religious philosophy course I’ve ever studied or taught. The abstraction is inescapable.
Redwan Moqbel: I think our difficulty is trying to interpret the spiritual in a practical fashion. Our society is so bent away from understanding the spiritual basis of our existence that when we want to resolve these issues, we think that maybe it’s a good decision for the courts to make. Religious communities need to take on the burden of nuance, to explain to their communities how we walk the spiritual path with practical feet.
Venkat Machiraju: You’re right, money is not the only factor.
Marion Magnusson: I want to make a comment about something else. The reality within a hospital setting is that there is a battle going on between clinical physicians and research physicians. The challenge for research physicians is to prolong life — they do not want to admit that there is death. There is also an incredible denial of death in our society. We hide our elderly. We have advanced directives. We have hospitals. We try to keep away from the reality that we die.
James Christie: Again, nuance. My childhood was dominated by my family caring for a dying person. I keep thinking of the phrase, “It takes a village to raise a child.” Frankly, I think it also takes a village to nurture a death. Yes, care facilities may not be an ideal place to die, but let me tell you, the drain on a family required to deal with a person for an extended period at the end of life, that’s a different kind of nightmare. And yet, I would agree with Marion on the whole business of denial. In congregational ministry, I was shocked by the number of times that families who were out of town would simply not come back for a service to mark the death of a parent, for example, but would simply arrange for a funeral home to ensure that a cremation and disposal of the remains was done, almost as you would order a book from Amazon.
Observer: Our time is up. I’d like to thank all of you very much for participating. It’s clear this is an extremely complex set of issues. It’s also clear that religious communities have an important part to play in the conversation about them. If I can draw one message for the courts and for politicians from what you’ve said today, it’s this: not so fast.
***
This story first appeared in The United Church Observer’s October 2012 issue with the title “End-of-life ethics: ‘A pioneer phase.’”