After a long day at work, Diane will often pick up fast food and drive to a nearby cemetery where she eats alone in her car.
Sitting among the quiet backdrop of gravestones, she braces herself for what awaits her at home. Her husband has psychotic depression and refuses to take his medication because he doesn’t like the side effects and, after one year on anti-psychotics, considers himself cured.
He was diagnosed 30 years ago, hasn’t worked since and spends most of his days obsessively snooping through Diane’s dressers and purses and reading her emails. When she’s home, he hovers over her, wiping down anything she touches with Lysol — part of his germ obsession.
“He knows no boundaries,” says Diane, who moved into her daughter’s bedroom three years ago when she left for university.
Diane (whose name has been changed) is in her late 50s, a short, stocky woman with washed-out skin and the faint smile of a battle-weary soldier. Years of putting up with her husband’s erratic and controlling behaviour have pushed her into a state of apathy. “I get overwhelmed thinking about how to untangle it all,” she says, shaking her head. “I just don’t have the energy or confidence anymore.”
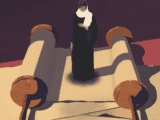
Marriage can be a road filled with unexpected curves but navigating that road with a partner who has a mental illness can add a whole other dimension to the journey. The stress can impact a person emotionally, physically, financially and socially and ultimately compromise his or her own health.
It’s something Diane knows only too well. “When you live with someone who is mentally ill, the whole environment becomes a bit ill but because you are so ‘in’ the situation you don’t realize how unhealthy it is,” says Diane.
The topic of mental illness has been gaining wider attention lately, with celebrities like Margaret Trudeau and Olympic athlete Clara Hughes telling their stories. With one in five people experiencing some type of mental illness or addiction problem, experts are pleased to see the discussion growing.
The person often missing from the conversation, however, is the partner or spouse of the ill person. Like Diane, spouses are directly affected by their partners’ illness not only because they shoulder the burden of caring for them, but also because they do the lion’s share of child raising and household chores.
Then there’s the loneliness. “That’s the hardest part,” she says. “I’ve lost all of my couple friends. They’ve told me they’d ask me over but they prefer that he doesn’t come because he makes them feel so uncomfortable.”
The Mental Health Commission of Canada outlined the significant burden placed on caregivers of someone living with mental illness in a 2013 report. It states that the nature of caregiving where a partner has a mental illness can generate substantial emotional, physical, financial and social hardships due to the “episodic and sometimes unpredictable nature of many mental illnesses.” Yet services for caregivers are “spotty and inconsistent at best (and often non-existent).”
Only a third of people with a mental illness receive the help they need and those who go without often rely on their spouses or loved ones for support; 75 percent of the spouses in a caregiving role are women.
“The mental illness has a direct impact on the spouse, and it can all fall back on them as the caregiver,” says David Butler, family counsellor with the British Columbia Schizophrenia Society. At the society’s Victoria branch, Butler facilitates a support group for the partners of persons with a mental health disorder. “There’s often exhaustion, resentment and guilt experienced by spouses. If there are children involved, there’s a feeling that they’re dealing with this on their own because they no longer have a partner to help them.”
The up-and-down nature of many mental illnesses makes caring for a loved one unpredictable. Persons with a mental health problem can have increased rates of hospitalization, are at higher risk of suicide and more likely to develop substance abuse problems.
What makes it even more frustrating for many spouses is that they’re often blocked from helping their partner. Under Canadian law, an adult’s health-care team cannot disclose any medical information, such as a diagnosis or treatment, without permission from that person. The laws were designed to protect privacy. However, some spouses say it leaves them in the dark — for example, if their partner refuses to tell them whether they’re taking their medication or following a prescribed medical plan.
“They have no power or influence over whether their spouse gets treatment,” says Sabrina Andrews, who facilitates the Family Support program at the Canadian Mental Health Association in Middlesex, Ont. “If the spouse [with mental illness] doesn’t recognize that they’re ill or doesn’t allow [their partner] to communicate with the doctor then [the partner] is left out of the whole treatment plan.”
Andrews provides support to people who have adult family members with mental illness, and says her clients are often fearful about things such as how their loved one’s reckless spending could impact them. “If my husband racked up a huge debt, I would have no power to take his credit card away but it would affect my credit rating and my financial situation,” says Andrews.
Maureen (whose name has been changed) knows all about those feelings of helplessness. Her husband was diagnosed with bipolar disorder but refused to accept the diagnosis, and convinced himself he could “fix” his symptoms with a rigorous fitness schedule.
Maureen stayed because they had a child together. Then he started acting more strangely. Maureen’s eyes widen as she describes the stressful months leading up to her husband’s breakdown: the excessive spending, erratic behaviour, mood swings. He bought a car without telling her, stayed out for nights without calling.
Seeing his behaviour escalate, she called the police, only to be told they couldn’t do anything. She felt she had no choice but to leave. Then, even though her husband refused to take his medication and was acting irresponsibly, she had to fight to get his visits with their child supervised. “There is no help for families of a person who have a mental illness,” says Maureen. “I felt like I was completely on my own.” u
Butler says many spouses are made to feel like they’re to blame for their partner’s problems. When Maureen told friends and family she was leaving, many expressed concern about how her “poor husband” would manage. Meanwhile, there was little support for her. “I told them I could only cope with so much,” says Maureen.
Because mental illness is an invisible disability, even medical professionals can be blind to the crisis. “If there’s a serious physical illness, you go straight to ER and you’re seen reasonably quickly,” says Butler. “Quite often in the mental health system, if the person puts on their best front, they don’t get the services they need.”
When support isn’t provided, Butler says many spouses go through an emotional transition that’s similar to the stages of grief. “First there’s the loss of a partner, lover and parent. Then the feelings of resentment and bitterness and anger build up. Then there’s the grieving at the loss of the partner they chose. Sometimes when it goes on long enough there’s also a loss of love.”
When a spouse feels like they’ve been transformed from partner to helpmate, a relationship can start to break down, says Butler. Those who leave often do so for the sake of the children. As Andrews says, “For many, it comes down to how you manage the mental illness of the spouse and still protect the children.”
Those who stay often do so for financial reasons. The ill partner may not be working and the household finances may have been depleted due to costly medications, hospital-related expenses and non-medical services.
Then there are others who stay for fear of being judged. “Some people endure and endure and endure until they become like martyrs,” says Andrews. “They feel like to leave somebody because they’re ill and to honour their own need for something better would go against their values.”
Andrews says among the couples who make it work, the deciding factor is whether the spouse with the mental illness is willing to take responsibility for his or her condition. That means following a treatment plan, practising self-care and allowing their partner to communicate with medical professionals.
That’s how Marion Gibson and her husband, John, say they’ve kept their marriage healthy. They’d been married 20 years when John had a psychotic breakdown in 2011. Marion was on a business trip in Ontario when she got a call from her husband at home in Victoria saying he’d called the police because he was convinced she was trying to poison him.
Marion describes the ordeal in her memoir, Unfaithful Mind, as “the worst period of my life” and says the breakdown came out of nowhere. John was eventually diagnosed as having a delusional disorder but it took years to find the right medication and dosage.
After John’s health stabilized, the couple sat down and wrote a step-by-step plan to follow in the event of another breakdown. “Because of the unique nature of John’s illness, he loses trust and confidence in me and in our marriage, and he really does not want anything to do with me,” says Marion. “If he doesn’t want to see the psychiatrist, then John has signed a form [allowing] me to discuss what is happening with the psychiatrist.”
Butler says open communication and working together with an element of trust and honesty is critical. He also helps couples establish a schedule that ensures both share the workload and both have time for self-care. That can be as simple as going for a bike ride or ensuring they’re getting enough sleep.
“Many people arrive here exhausted, and they’ve gone into bunker mode where they don’t want to make any big changes. They’re frozen from being in a state of crisis,” says Butler. “We try to untangle that ball of wool.”
For Diane, that ball of wool has so many knots she doesn’t know where to start. She’s found her own ways to cope, even if means sitting alone in a cemetery. She sometimes allows herself to think about an exit plan: moving west to be close to her parents, far away from the madness that is her marriage.
With that faint weary smile she says, “The danger of living with a mentally ill spouse is that you lose sight
of normalcy and get sucked into the chaos.”