Their stories made headlines in 2008. Cathy Cormier, a 50-year-old gallstone patient, spent two days lying in a gurney pushed up against the check-in desk of a Halifax emergency ward. She was expected to stay there until more hospital beds opened up. Brian Sinclair, a homeless man and double amputee, died of preventable bladder and abdominal infections sitting for 34 hours in a Winnipeg emergency room. Antibiotics and a simple catheter change would have saved the 45-year-old’s life.
The queues for health care across the country have become a common and alarming sight. Access to family doctors and emergency services has worsened over the years, partly due to shortages of doctors and space. As a result, Canadians’ faith in a publicly funded health-care system — best known as medicare — has been rudely shaken, leading some to call for a mixed public-private system.
You may unsubscribe from any of our newsletters at any time.
Supporters of this two-tier system, which already exists due to the surge of specialty clinics, say that increased competition from the private sector would cure wait times and force the public system to become more efficient. But medicare advocates, including United Church leaders, view private for-profit clinics as a threat to the Canadian health system itself. They argue that outright privatization would draw many of the best doctors out of the public system and drive up the wages of medical professionals. They believe a just society includes the equal treatment of sick people. But above all, they insist that the current system is on the mend — so why dismantle it?
Every year, Canadians make 14 million visits to emergency departments, according to Statistics Canada. They frequently call on their family doctors, too. A recent Pollara survey showed that most Canadians believe the health-care system needs major repairs or a complete overhaul. But they are conflicted about the private sector’s role in health care.
Like it or not, there are now 89 private for-profit clinics doing surgery, MRIs and CT scans across the country. These “boutique” clinics operate despite the Canada Health Act’s prohibition of private for-profit health care.
Conservative think tanks, such as the Fraser Institute, clearly like the idea. The organization has long dismissed the current system as a “single-payer health insurance monopoly” that doesn’t cover many advanced medical treatments. It argues that people should be free to buy private health insurance, as they do in countries such as Sweden and Australia.
The Canadian Medical Association, the country’s main lobby group for physicians, also supports access to private-sector health services in circumstances where patients can’t otherwise get timely access to care. The association’s president, Dr. Robert Ouellet, runs several private radiology clinics in Quebec. He argues that Canada’s health-care costs have quadrupled in the last 20 years; the doctor-to-patient ratio has plummeted; and by 2011, the number of Canadians over 80 will have jumped by 43 percent. In the face of a shortage of operating rooms, he questions the logic of banning surgeons — who provide 90 percent of their services in a hospital — from performing five to 10 percent of their surgeries in a private clinic. “Canadians must wake up to the key role private health care can play in relieving the country’s ailing public system,” he told the Globe and Mail last summer.
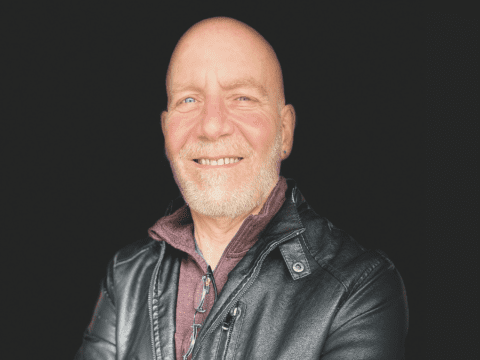
Until recently, retired United Church minister Rev. Bill Jay carried out The United Church of Canada’s health-care advocacy through the Canadian Council of Churches’ Ecumenical Health Care Network. He acknowledges that two-tier health care is already here but strongly urges “the need to carefully manage it.” He warns, “The moment people start paying private premiums, they’re going to want to be exempt from paying for public health services. When doctors, nurses and technicians are poached by private clinics, more health-care practitioners will follow. It could have a siphoning effect.”
United Church Moderator Rt. Rev. David Giuliano, who has spent almost two years undergoing cancer treatment, says private health care “seems to increase the likelihood that those at the bottom end of the care system will get sub-standard treatment.”
It reminds Giuliano of the separate-but-equal schools for African-Americans in the United States. “I don’t think anyone will tell you that those schools were funded in the same way Anglo-Saxon schools were,” he says. “I can’t imagine the Canadian health-care system won’t go the same route if we insist that people with their pockets full of money can buy their way out of the system that is intended to serve everybody. From a theological starting point, those who are wealthy have a special call to those who don’t.” He adds, “True, we no longer live in a culture where that’s the basis of any argument, but as a church, we need to move out of that reality and lend our voice to the national conversation about health care.”
It’s been more than six years since former Saskatchewan premier Roy Romanow released his report on Canada’s health care. His 47 recommendations — which included reorganizing family doctors into teams, computerizing health records and developing a national pharmacare program — were heralded as a blueprint for the 21st century. But up until now, little has been done to act on the report. Romanow now wonders what his 18-month, $15-million commission accomplished. He told reporters last June that the Canada Health Act is “almost becoming a dead letter of the law.”
A major concern now is the “enforceability” of the Health Act, according to Raisa Deber, a professor of health policy at the University of Toronto. “Your doctor does not work for the government. Your doctor is a small business entrepreneur who only bills the government,” she says. “When we’re talking about increased privatization of health care, I have doubts about a model that is based on the assumption that people are going to be altruistic enough. Think about it. If I’m a venture capitalist in the field of medicine and I have this situation in which people are willing to buy their way to the front of the queue, why would I try to lower the number of people on my wait list?”
While the debate over Canada’s system rages on, the federal government’s 2007 budget offered more than $600 million to encourage provinces and territories to implement wait-time guarantees by 2010.
Bill Jay continues to represent the church on the board of the Canadian Health Coalition, which aims to safeguard the legacy of universal health care. “[Today’s medicare] still fulfils the vision of its founders that it would be there when we need it, irrespective of our ability to pay,” he says. “Whether you are paying no taxes as a person with a disability or a CEO of a prosperous firm, you have an equal chance of getting prompt treatment.” But Jay concedes that there is plenty of room for improvement, and that much more can be done to accommodate patients like Cathy Cormier and Brian Sinclair.
“The prescription for Canada’s ailing health care is to fairly allocate the resources that are there to make sure that the Canada Health Act and the public system as we know it do not erode through double-dipping,” he says. “This really is an issue that affects all of us and not just the ne’er-do-wells. It’s like the old adage from the Book of Corinthians, ‘If one member suffers, all members suffer together.’”
***
This story first appeared in The United Church Observer’s January 2009 issue with the title “Condition critical.”