This interview is the second in a six-part series about rethinking the police. A new article will be posted every Wednesday.
Regis Korchinski-Paquet. D’Andre Campbell. Andrew Loku. These are just three Black lives lost in Canada after police were called during a mental health crisis. The Toronto Police Service alone responds to about 30,000 mental health calls a year. Despite the frequency, critics say police are ill-equipped to manage them. Too often, those in crisis — particularly Black and Indigenous people — are dying at the hands of police.
Donna Alexander is a social worker at the Centre for Addiction and Mental Health (CAMH), which is calling to end mental health checks by police. Alexander has worked for 15 years with Black youth dealing with mental illness and addictions, and sometimes she has to call police to assist with her clients. Alexander spoke to Sadiya Ansari from her home in Toronto.
Sadiya Ansari: What are the barriers to accessing mental health care for Black youth?
Donna Alexander: If you are a person that is experiencing mental health issues, it’s really difficult to navigate the system. It’s designed for the powerful. The people who need to access the system are poor, vulnerable and marginalized. I have clients who are afraid of places like CAMH — it’s intimidating. So what usually happens is that people wait until it’s too late, when they’re so sick that the police have to take them to the hospital. It’s traumatizing because now they’ve been handcuffed, placed in the back of a police car, and they’re confused.
SA: You’ve acknowledged that it’s not your first choice to call the police, but sometimes it’s the only choice. What is it like when you have to make that call?
DA: It’s anxiety-ridden. I’ve been working with a young Black man from the time he was 17, and now he’s 27. The first time we called the police for assistance was when he was 18. We had to call that night because he was literally starving himself to death — he thought people were poisoning his food. When the police came, there were eight of them, and they took him down. He was crying and screaming and fighting. And by the time they left, the entire staff was in tears. It was so traumatic for everybody to witness. He went to the hospital, and he was treated. He started eating again. And then he was released from the hospital. But ever since they released him, he stopped taking his meds and he’s been on the streets. To this day, because of that first traumatic experience, I’m always hesitant to call the police.
SA: What do your clients, and you, fear when you call the police?
DA: The fear really is that they’re going to be killed by the police. This is why I’ve actually had to say to dispatchers, “My client is very sick, has schizophrenia and is not on his meds. I’m calling you so that the police can take him to the hospital. I’m not calling you so the police can go there to shoot and kill him.”
SA: What goes through your mind when you hear about cases like Regis Korchinski-Paquet, where the police were called to help a person in crisis and that person ends up dead?
DA: Every single time, I’m thinking: “What kind of society am I living in that we allow this to happen to vulnerable citizens?” And I cannot help but think — and people don’t like it when I say this: “Is it because these are mostly racialized, marginalized people? Would this be happening if these were white people?”
More on Broadview:
- This retired cop wants to see police culture transformed
- It’s time for Canada’s statues to fall
- 5 resources to help you become a better ally to Black people
SA: What tips do you have for people who aren’t social workers and who may have to call police to help a loved one in mental distress?
DA: I have to prepare Black parents. When you call the police, before you let them in the house, meet them outside the door with the door locked and say to them: “My child is this age; this is what’s happening; my child is not violent; there are no guns, no knives.” Humanize the child. They shouldn’t have to do this, but I have to prepare them.
When the children and their parents are white, the parents do not experience this. Instead, I hear things like, “The police have been so understanding; the police saw cocaine sitting on the table and pretended they didn’t see it; the police were so co-operative.”
SA: CAMH recently called for police to stop doing mental health checks. What’s your preferred alternative?
DA: A good alternative is to have trained mental health crisis workers that have expertise in de-escalation. Even if there is police backup, I don’t think police officers should show up in uniforms because a uniform triggers people. When you are sick, when you don’t have capacity and you see police officers, you think they’re going to take you to prison. You’re not thinking the police officers are here to take you to hospital. And so you’re confused as to why the police officers are there to take you to jail. A lot of times, this is how things escalate.
I cannot even believe that the community has to be advocating for crisis workers. But I understand why, in terms of the power of the police union, the lack of political will and the indifference to marginalized, vulnerable people. And systemic racism — the fact that some lives matter less than others.
SA: In a crisis, what kind of approach works better than what you see now?
DA: I saw on TV that Camden, N.J, terminated all the officers, redid the hiring process and retrained them. There was a scenario where a man in a fast-food place had a knife, and he was waving it around, threatening people. The police surrounded him, and they managed to get him out. Then they just followed him down the street for like five blocks. They kept their distance and followed him, so they were able to arrest him without an incident.
What’s happened with police services now, it’s almost as if officers want to get the encounter over with as soon as possible. That’s when you shout: “Drop the knife! Drop the knife!” But if your goal is to engage, then you don’t even focus on the knife. That’s not the way to do it.
When you do crisis work, you are trained: however long it takes is however long it takes. A part of that process is to wear down the person. The person gets tired after a while. When you get tired, you have the option to tap out and have someone else take over. Your job is to exhaust them.
You start engaging them: “Oh, Mrs. So-and-so, Mr. So-and-so, did someone do something to upset you?” It gives you the chance to gauge capacity as you’re talking to the person. If they’re responding and you can see that they’re having delusional thoughts, you know what to do.
SA: What do you hope will come from the public conversation on reimagining the purview of police?
DA: I’m hoping that there will be police reform and that funds will be reallocated to provide 24-hour crisis support staff that can go out and meet this need. Because clearly what we are doing is not working.
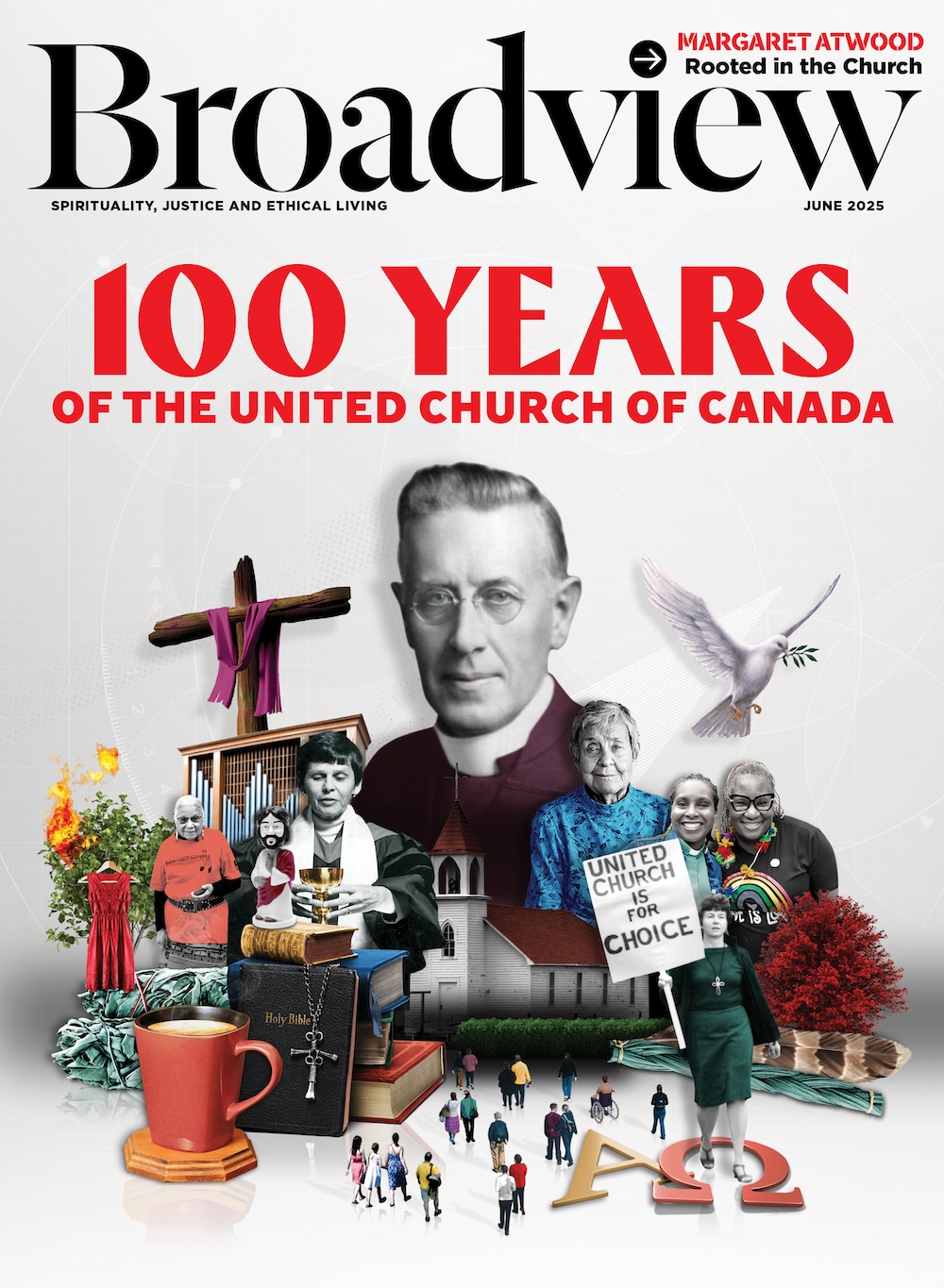
This interview first appeared in Broadview’s October 2020 issue with the title “The system is designed for the powerful.”
***
Sadiya Ansari is a writer in Toronto.
I hope you found this Broadview article engaging. The magazine and its forerunners have been publishing continuously since 1829. We face a crisis today like no other in our 191-year history and we need your help. Would you consider a one-time gift to see us through this emergency?
We’re working hard to keep producing the print and digital versions of Broadview. We’ve adjusted our editorial plans to focus on coverage of the social, ethical and spiritual elements of the pandemic. But we can only deliver Broadview’s award-winning journalism if we can pay our bills. A single tax-receiptable gift right now is literally a lifeline.
Things will get better — we’ve overcome adversity before. But until then, we really need your help. No matter how large or small, I’m extremely grateful for your support.
Jocelyn Bell
Editor/Publisher











I agree with the idea that police are not particularly trained to deal with mental health issues. And when they are called to such situations they often handle them inappropriately.
And I entirely agree with Donna Alexander’s idea of providing “24-hour crisis support staff that can go out and meet this need” of responding to mental health crises. Such support would be better for everyone, including the police.
Donna Alexander is DEDICATED, EDUCATED, and is truly doing god’s work. She has gone above and beyond to help my daughter. Tirelessly giving more of herself than any worker we have ever had – and we have had approximately 6 different workers who eventually gave up.
Worker(s) gave up and or left because they could no longer see the PERSON struggling with her mental health issues and addictions. YES social workers have a very high rate of burn out and rightly so given what they do for others. I have MAD respect for Donna – as a Human Being, Person of Colour and Woman. Thank you from the bottom of my heart!