Flu epidemics, logging accidents, bear attacks, emergency surgeries and the life-saving practice of family medicine punctuate the 124-year history of United Church hospitals on the central coast of British Columbia. What may be its last chapters are being played out with much less drama.
The Vancouver Coastal Health authority announced last summer that by next June, it will take control of both the R.W. Large Memorial Hospital in Bella Bella and the Bella Coola General Hospital. It currently provides the hospitals’ provincial funding, as well as their IT and payroll services.
That leaves the United Church Health Services Society (UCHSS), a non-profit organization formed in 2008, operating only the Wrinch Memorial Hospital in Hazelton, B.C. This 20-bed hospital works through the Northern Health authority, based in Prince George, B.C. But without funding from all three hospitals to pay the UCHSS’s two full-time and three part-time employees, Wrinch Memorial’s days may also be numbered.
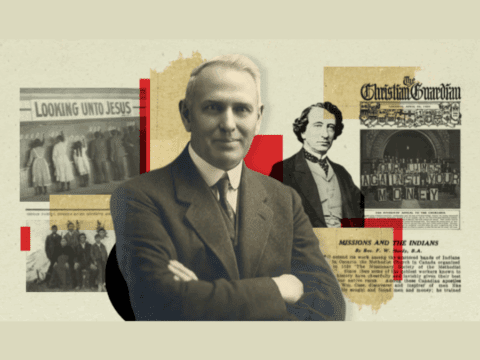
At one time, the United Church owned and staffed up to 32 hospitals and medical clinics in Newfoundland, Ontario, Manitoba, Saskatchewan, Alberta and British Columbia. It was an era when public health-care funding was scarce or non-existent, and many rural or remote communities lacked proper medical services. The work was financed and managed by the Methodist Mission Society, then the United Church Woman’s Missionary Society (later the UCW) and the Home Missions Board (later the Division of Mission in Canada).
Well into the 20th century, the church’s medical and missionary work went hand in hand. But just as many one-time “mission fields” are now congregations, most hospitals have been handed over to secular health authorities.
By 1939, the number of United Church-run hospitals had dropped to 24. This number plummeted to 10 in the late 1960s, and to four by the early 1990s. Today, the two remaining United Church-affiliated hospitals are Wrinch Memorial and the Lamont Health Care Centre. Located northeast of Edmonton, the Lamont centre is funded and operated by Alberta Health Services — the province’s single health authority — but the United Church names the majority of the hospital’s board of directors.
Improvements in transportation and infrastructure have brought better health care to much of rural Canada, but large swaths of British Columbia’s central coast remain difficult and expensive to reach. It’s about a three-and-a-half-hour drive from Prince Rupert to Hazelton. Bella Coola and Bella Bella can only be reached easily and quickly by air. The logistics of providing medical care on the coast remain daunting.
As a missionary enterprise, B.C.’s west coast had plenty of appeal, with myriad opportunities for doing God’s work in the shadow of the mountains, among First Nations and others.
Rev. Dr. Peter Newbery did a good job of persuading doctors and nurses to take up the adventure offered by the B.C. hospitals. Starting out as a young fly-in pilot-preacher in northern B.C., he took medical training, then returned to serve as a physician and United Church health services director for 35 years. After retiring and working as a medical educator, he’s back at Wrinch Memorial as part-time medical director.
In recent years, Newbery’s recruiting efforts have faced intense pressure from national doctor and nurse shortages. He says he’s always tried to hire “people who have a sense of mission and calling.” Failing that, he’s been able to offer signing bonuses of up to $100,000, provided by the provincial government.
Newbery says it’s become harder to find physicians with that particular sense of mission. A church-wide appeal sent to Presbyteries and congregations last year drew little response. Most medical school graduates want big salaries, regular hours or even part-time hours, and minimal time on call, he says. For nurses, the hospitals have increasingly turned to hiring agencies that provide short-term help.
With staff shortages, it’s been a struggle to ensure shifts are covered at all three hospitals. Last summer, medical staff pushed the endurance envelope, with doctors taking 24-hour on-call shifts every second or third day for weeks at a time. In a hospital annual report, Newbery called the short-staffing “a thoroughly unacceptable situation which . . . seriously affects our day-to-day attention to the broader patient care needs in the community.”
So why does Vancouver Coastal Health — a largely urban health authority with a $3-billion budget, 13 hospitals and 13,000 staff — want to do health care on the remote central coast?
One reason is simplification. Although VCH currently funds the two United Church hospitals, local community councils advise the hospitals, and the board of the United Church Health Services Society oversees them.
This fall, the newly minted First Nations Health Authority (FNHA) took over management of Health Canada’s programs for B.C. First Nations people. VCH had already signed a partnership agreement with the FNHA, and the UCHSS supported it. But in the alphabet soup of health-care governance, funding and management, the United Church was one manager too many.
With VCH and the FNHA working together, including the United Church in the mix “was like having three on a date,” says Dr. David Arnold, a semi-retired Bella Bella physician. “I think they wanted to ditch us.”
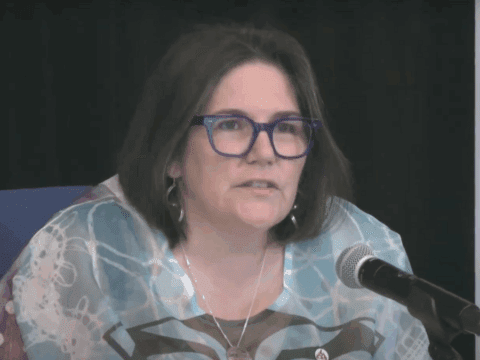
The provincially funded health authority had been highlighting its relationship with the new First Nations authority, says Health Care Services Society CEO Mary Jean Morrison, and the United Church hospitals may have been caught in “a bit of a political squeeze play.”
As well, the UCHSS had run up annual budget deficits of $100,000 to $200,000 for several years, adding up to $2.14 million. UCHSS staff and board members blame the shortfalls on inadequate funding. But the UCHSS is responsible for paying those deficits, according to its agreement with the health authority.
Whether or not that happens depends on negotiations and exchanges of property and other assets during the VCH takeover of Bella Bella and Bella Coola hospitals, says Jon Jessiman, B.C. Conference’s representative on the UCHSS board.
As the hospitals’ new operator, VCH wants to avoid future budget deficits. It already has $152 million in accumulated operating deficits on its own balance sheets and hopes to help the central coast hospitals save money through bulk purchases of medical supplies, information technology support and other services.
When the first doctors and nurses arrived along with missionaries on the remote B.C. coast, says Jessiman, “it was never intended that the United Church become a long-term provider of health care.” So, despite a lack of prior consultation and notice, the UCHSS wants to make the transition to VCH as smooth as possible.
The United Church plans to transfer land — given to the church by Aboriginal people for hospital work — back to First Nations. The UCHSS has also agreed to manage the medical clinics operated along with the hospitals for another year.
Many people won’t notice the change right away, says UCHSS chair Lynn Nelson, a longtime Bella Coola hospital council member. “What is the value-added of having the United Church in [Bella Coola] and in Bella Bella? It’s the local input, the history. It’s not really a tangible thing.”
Cynthia Breadner, a theological intern and minister at Bella Coola’s Emmanuel and Augsburg-Mackenzie United churches, says many people are “in grief and in shock” but have “an overall concern for losing the hospital — losing services.”
That fear may now extend to Hazelton. Ray Jones, chair of the United Church’s national Aboriginal Ministries Council, lives in Gitsegukla, B.C., about 30 kilometres southwest of Wrinch Memorial Hospital, and sits on his village’s health council. The United Church hospital has a long history, he says, and programs in partnership with communities are working well. Big health authorities, on the other hand, “are always cutting corners.” As for the future of the Hazelton hospital, he says, “We’ll see what happens.”
Newbery is not hopeful that the UCHSS can continue with Hazelton as its only hospital site. “I do see the writing on the wall,” he says. For now, though, the focus is on easing the transition and honouring the United Church’s health-care history.
Rev. Bob Burrows is a United Church minister who worked on the B.C. coast and wrote Healing in the Wilderness: A History of the United Church Mission Hospitals in 2004. He returned to Bella Coola this year as a retired supply minister and heard “overwhelming support and gratitude for the hospital and for the United Church involvement.” He hopes to hear the same support and gratitude for the Vancouver Coastal Health authority sometime in the future.
***
This story first appeared in The United Church Observer’s December 2013 issue with the title “Condition critical.”