Between flu epidemics, grizzly bear attacks and emergency appendectomies, there have been many life-saving moments at United Church hospitals. Doctors and nurses have braved high seas aboard mission ships, journeyed into remote areas on horseback and co-ordinated back-country helicopter rescues.
But today, after almost 120 years, the church’s less dramatic work of community-based preventive health care and a strong commitment to rural medicine may prove to have the most enduring impact. The church’s hospitals and medical facilities are greatly reduced in numbers and profile but nowhere near extinction.
At first glance, the trend line doesn’t look good. Over the years, the United Church has owned and staffed about 30 hospitals and related medical clinics in Newfoundland, Ontario, Manitoba, Saskatchewan, Alberta and British Columbia.
By the early 1960s, the number was down to 10. Today there are four. The medical work used to be well known in church circles. Its superintendent or director was on General Council staff as recently as the late 1990s. Today, the remaining hospitals and accompanying clinics, three in British Columbia’s central and northern coast and one in Lamont, Alta., get no church funding but are still legally owned by the United Church. Health and nursing consultant Heather Clarke diagnoses a “critical lack of knowledge . . . among United Church people.”
The church is now more of an ongoing presence in the hospitals’ governing structures than in their operating rooms. And public funding leads to a more secular approach to delivering health care. According to Dr. David Arnold, the medical director of United Church Health Services in British Columbia, it leaves the church asking, “What does Christian service look like when we are not evangelizing in the strictest sense of the word? We’re not going out to convert the heathens anymore.”
To Clarke and others, Christian service looks something like the church’s longstanding commitment to social justice. “It underlies what gets done,” she says.
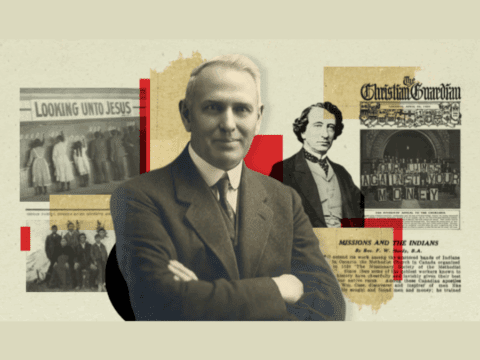
In the early days, the United Church’s hospital work was very much a product of the evangelizing zeal of its precursors. The first Methodist hospital was set up in Port Simpson at the behest of renowned West Coast missionary Rev. Thomas Crosby. Later, notions of service and helpfulness, plus the promised adventure of life on the edge of the wilderness among Canada’s First Nations, replaced saving souls as the motivation for doctors and nurses who chose church work over secular jobs.
“I wasn’t there as a missionary,” says Judy Wass, a nurse and assistant administrator who worked at Wrinch Memorial Hospital in Hazelton, B.C., for 25 years. “I was there to be part of a community and to get to know people. I was not there rescuing anybody. I never even talked about being a Christian.”
Some of the church’s best-known physicians, including former moderator and China missionary Dr. Bob McClure and Dr. George Burgess, a longtime Angola missionary, also worked in Canadian church-run hospitals. They were not without fault — one hospital in British Columbia had segregated wards for Indigenous Peoples during the mid-1950s, and a church doctor was convicted and jailed for sexually abusing children in Newfoundland in the 1980s. For the most part, though, the hospitals provided high-quality health care to remote and isolated communities that had few other alternatives.
Dr. Don Watt of Vancouver spent virtually all of his medical career with the United Church, working as a doctor in the Queen Charlotte Islands and Bella Coola, B.C., then as superintendent of United Church hospitals and medical work for 36 years before retiring in 1989. His father was a United Church minister, but he credits his brother, also a medical doctor, for giving him “a sense that if you have some wisdom and training, you use it for the betterment of your fellow human beings.”
Watt and his successor, Dr. Peter Newbery, used United Church connections to recruit medical personnel. Watt would tell them, “These are great areas and you’ll never be the same after you’ve been up there. And besides, the fishing is good.”
With the advent of medicare, government funding has increasingly paid for United Church hospitals and health facilities. And as communities developed, they’ve wanted more control.
By the 1980s, the United Church connection was severed in B.C. locations such as the Queen Charlotte Islands, Burns Lake, Ocean Falls and Stewart, as well as in Cold Lake, Alta., and Eriksdale, Man. In the ’90s, the Baie Verte, Nfld., hospital was handed over to a local authority.
Along with Watt and Newbery, a few longtime staff, including Dr. Phil Muir and Dr. Ray McIlwain, helped the church’s remaining B.C. facilities survive and thrive. “Everybody was there to be a good physician and would stay around until the job was done,” says Muir, who is retired but regularly lends his computer expertise to Wrinch Memorial.
Like all rural and isolated medical facilities, United Church hospitals have found it harder to recruit physicians during the last two decades. Newbery’s response was to strengthen the B.C. hospitals’ relationships with the University of British Columbia’s medical school, using the hospitals’ status as accredited teaching sites to bring in medical residents, interns, nurses and physiotherapists. The program created a pool of talented doctors and nurses often open to short-term assignments.
By 2002, with responsibility for church medical work handed off to British Columbia and Alberta and Northwest Conferences, Newbery and others wondered if it was time to transfer the last of the B.C. hospitals to newly created regional health authorities.
B.C. Conference formed a three-person commission to look into the idea. With the three facilities in question functioning as much more than acute-care hospitals (each has a clinic and pharmacy and offers unique services such as teleconferenced psychiatry and psychology), commission member Heather Clarke says, “It was clear from everybody that they wanted the United Church to stay involved.”
Jim Angus, a school administrator, active United Church layperson and member of the Gitxsan First Nation in Kispiox, B.C., says church hospitals and clinics are “part of the family” in the communities they serve, where Indigenous Peoples make up as much as 60 percent of the population.
Under Alberta and B.C. law, church-affiliated hospitals are required to have local boards. The United Church appoints some members, but most are drawn from the community. In B.C. that means Indigenous Peoples have considerable input into how health care is delivered locally. New agreements between various B.C. First Nations and the recently created United Church Health Services Society aim to strengthen co-operation between church and community.
In Alberta, Lamont’s local board helps the hospital deal with ever-changing provincial health care structures. Conference’s advisory committee chair Debra Morris says staff and volunteers “want people in the church to know they exist, that they live out their call to healing in a very concrete way.”
In B.C., too, there’s a renewed recognition of what health services medical director Dr. David Arnold calls “United Church principles.” A values statement for physicians asserts, “God intends wholeness for all people, and . . . our role is to assist and enable individual and community wholeness.”
The communities the church hospitals serve are not as isolated as they once were, but face other challenges. According to Health Services Society CEO Glen Timbers, Upper Skeena, served by Hazelton, has the “worst socio-economic rating” of any health area in the province because of crime, economic hardship and youth and children at risk. In Lamont, Alta., downwind from petroleum upgraders, air quality and its effects on health are a concern. Timbers hopes renewed connections with the United Church will result in “leadership in developing management and community processes.” In other words, figuring out better ways to improve health care in isolated and rural areas.
It sounds like a 21st-century version of what first drew church doctors and nurses into the Canadian wilderness in the first place. And it may just help give United Church medical work a new lease on life.
***
This story first appeared in The United Church Observer’s November 2008 issue with the title “Healing in the hinterland.”