Three years ago, Susana Meza, a vivacious Venezuelan artist living in Toronto, was incredibly frightened about the future. She was participating in a substance abuse recovery program at a local women’s centre. It was her third attempt at getting sober from alcohol, which she’d been given since she was eight months old.
“I thought that my life was over, that I was never going to be able to have fun, go to the places I liked or be with the people I enjoyed being with because there were always substances there,” Meza told me over Zoom in January, surrounded by in-progress paintings the colour of the sky at dusk. “Then this woman came [to the centre] as a peer support worker. The fact that she had this vibrant and genuine joy for life was so inspiring. It was a dream come true to hear that someone could go through life without coping [by using substances] and still grasp on to happiness.…That gave me hope, and that hope turned into the work I now do.”
Today, Meza uses her recovery to inform her work as a mental health peer supporter and artist facilitator at organizations like Toronto’s Centre for Addiction and Mental Health (CAMH) and Workman Arts, an arts organization promoting greater awareness and understanding of mental illness and substance use disorder. She’s also the founder of Reclaimed Arts, a series of social and community art projects that support people with lived experience of mental illness and substance use, survivors of gender-based violence, and trans youth.
Peer Support Canada describes peer support as emotional and practical support between an individual and a trained and paid peer supporter who share a common experience, such as a mental health challenge. The work involves a lot of active listening to others who are struggling with their mental health, offering advice or empathy informed by the peer supporter’s experiences, and encouraging people to use their unique strengths to support their recovery. Peer supporters don’t treat mental illness but model how to live with mental health challenges effectively.
Peer work can happen in conjunction with or separately from clinical treatment, and may be one-on-one or in group settings. It’s primarily available through mental health organizations, but peer support roles can also be found in some institutions like hospitals or universities. Required experience or accreditation varies widely. Meza, for example, holds certifications in emotional CPR, standard mental health first aid, mindfulness practice and peer support core competencies.
Peer supporters instil hope and promote recovery in the people they work with through leading by example. Expanding these programs could be one of the solutions to surging mental health needs in Canada. Unfortunately for Meza and others like her who bring so much heart and soul to their work, the peer support sector is fledgling. If it’s scaled up without careful consideration, it risks repeating the systemic harms it seeks to alleviate during a time when the country needs peer support most.
Meza believes peer support has deep roots in the history of our species. “When our ancestors gathered by the fire, they did peer support. It’s taking that ancient knowledge and bringing it back to try to be there for each other.”
Within the western mental health system, peer support dates back to the late 18th century, when Bicêtre Hospital in Paris began to hire former patients as hospital staff. In a 1793 letter, Jean-Baptiste Pussin, the facility’s governor and himself a former patient, wrote that recovered patients were “better suited to this demanding work because they are usually more gentle, honest, and humane.”
In Canada, models of peer support have been available since at least the early 1940s, when Alcoholics Anonymous started crossing the U.S. border. Following Canada’s deinstitutionalization movement in the 1960s, which advocated for people with mental illness to live in community, the country’s first peer-run support organization, the Mental Patients Association of Vancouver, was founded in British Columbia in 1971. By the 1980s, former patients in Toronto launched a number of community initiatives like drop-in centres, second-hand stores and the magazine Phoenix Rising. During this period, the role of the peer supporter became more formalized within health policy but was met with mixed responses and often fell to the mercy of budget cuts.
While provinces and territories are beginning to incorporate more peer work into their mental health services, availability is largely dependent on where a person lives. A 2016 report by the Mental Health Commission of Canada found significant variation in the development of peer support across the country. Ontario has about 60 programs run for and by people with mental health challenges, and the Ontario Peer Development Initiative serves as a provincial umbrella organization. However, growth hasn’t been consistent: since 1991, only 18 initiatives have been started in the province.
In the North, the Yukon funds peer-based initiatives like the Blood Ties Four Directions Centre, and the Northwest Territories recently launched the Addictions Recovery Peer Support Fund, which communities can apply to for funding for their own peer-led support programs. Manitoba invests in the Peer Connections program, and last summer British Columbia unveiled Where We Are At, a provincially approved training curriculum for peer support workers. But pockets of the country, like Prince Edward Island, still offer limited peer support services. The province’s very first peer support training program began last autumn.
Some studies show that peer support services are equally effective to similar services provided by non-peer professionals and have a more positive impact on levels of hope, empowerment and quality of life. The Mental Health Commission of Canada found the benefits of peer support also include a reduction in hospitalization rates, isolation and symptom distress, and lower costs for the health-care sector.
This last point is significant: the economic burden of mental illness in Canada is estimated to be $51 billion per year. In a 2005 study conducted in Ontario, people who received peer support were discharged from the hospital an average of 116 days sooner than those who didn’t, resulting in considerable savings. A 2018 Psychiatric Times article illustrates that peer support is a “win-win situation for resource-strapped systems”: patients receive support that instils hope and assists in their recovery journey, people with lived experience of mental illness are employed in roles that support their recovery, and the mental health system gains an effective and trained workforce.
“I’ve seen it happen,” says Allison Dunning, national manager of Peer Support Canada. Like everyone I spoke to for this story, she comes to the sector with her own lived experience. “When people are feeling really stressed out, they’ll call a peer supporter instead of going to the emergency department.…If peer support isn’t there, then the only option is hospital, and is that the best use of the hospital’s resources? Probably not.”

Peer support can feel more accessible to people in crisis and help connect them to other services. Erica Ruth Kelly, peer initiative co-ordinator at Stella’s Place, a Toronto-based treatment centre for young people that offers peer support as a cornerstone of its programming, experienced this benefit herself. She has spent over 20 years receiving different types of clinical counselling for her mental health. She says there is something missing from all of it, which she didn’t realize until she worked with a peer supporter. “What I experienced was the difference between somebody who was listening with their brain versus a peer support worker who was listening with their body and their heart.”
Yet as mental health needs increase, this vital component of recovery is often overlooked or underfunded in Canada. Across the sector, peer workers face challenges related to their precarious status, including a lack of payment, unclear career trajectories, poor access to support, and not being accepted by the wider mental health workforce.
Don Vaillancourt, a French-Canadian artist and musician, works as a peer supporter at Workman Arts and The 519 in Toronto. Like many in the sector, Vaillancourt struggles with getting the support they require to do their job effectively. Peer supporters aren’t meant to treat mental illness, yet they’re sometimes compelled to respond beyond their training. Vaillancourt and I spoke following a challenging week when they had tried to support a person in crisis while ensuring the three others in the support group weren’t triggered or neglected. “Support people are not psychiatrists. We’re not psychotherapists,” says Vaillancourt. When a peer worker is overwhelmed, it’s not always clear who they can go to for help. Vaillancourt would like to see “a support group for support workers monitored by a psychotherapist.” They add, “A lot of peer support people I’ve worked with had to take a term off. People are burning out.”
Vaillancourt’s concerns are echoed by other peer workers. “We have a really great ability to have a really fluid role, but there can be challenges around peer supporters feeling not entirely clear on what is within their role,” says Paige Lougheed, provincial peer support co-ordinator for Foundry, a network of integrated health and social services for young people in British Columbia. “Another thing we’ve seen [is that] it can be hard to have that next step after you finish a youth peer support role.…If we’re really going to talk about peer support as its own discipline and its own field, there should be career opportunities. There should be that next step available for peer support workers to see a path for themselves.”
Amber Scott, a peer support worker with Youth Wellness Hubs Ontario, an organization I received an honorarium from to contribute to a peer support training curriculum for youth, believes one of the ways the country could bolster peer support programs is through official certification for peer supporters. “Peer support training programs that are accredited and certifications that are recognized in the same way clinical certifications are recognized…are really important,” she says. Peer Support Canada offers the only nationally recognized certification program, but it is not a training program, which are usually provided at the provincial or community level.
Some of the challenges peer supporters face in their roles stem from the friction around fitting grassroots, person-centred healing into more rigid clinical settings like hospitals or out-patient facilities.
Chyrell Bellamy, an associate professor of psychiatry at Yale University and director of the Yale Program for Recovery and Community Health, believes fear is a factor too. Peer support “confronts the whole clinical establishment,” she says. She points to a 2019 Psychological Services article in which one participant noted, “I heard others say that by hiring peers, they were letting the patients run the asylum.” Another interviewee had their role undermined when a doctor told their co-workers not to listen to them because they had their own diagnosis. This gels with research that found, in many western contexts, lived experience roles are not accepted by the wider mental health sector.
“When we do see peer support embedded in the system, it’s more around fitting in,” says Bellamy. “It’s not transformative because nothing changes.” Instead of imagining how peer workers might challenge or expand the clinical paradigm, “you just plop someone in and you hope everything happens.”
Research that Bellamy contributed to has warned that authentic peer support work can be compromised when peer workers are put into “para-clinical” roles. She points to hugging policies as an example. In clinical psychology, there are ethical guidelines around hugging or touching patients. “But if you have a peer supporter, do they have to have those same policies or should we develop new ones that are really human-centred?” she asks. “If touch is one of those ways we connect with someone, why are we placing these false boundaries and ethical values to peer support that are similar to clinical ethical boundaries?”
Trauma-informed training that maintains the spontaneous and holistic nature of peer support can help clarify roles and ensure peer supporters aren’t misused, says Bellamy. She also advocates for peer support supervisors who are trained in the discipline as opposed to coming from more clinical backgrounds. While she concedes that standardization across the sector would place more value on peer support work, she warns it isn’t necessarily the best path forward. “With that comes more oversight and regulation,” Bellamy says. “The more of that you have, the more bureaucracy you’re walking into and trying to do peer support in that space.” In the 2019 Psychological Services article, some peer supporters described being in roles that positioned them as second-rate team members with less of a voice, an example of professionalizing gone awry.
“It’s key not to fall into a trap of over-standardizing or over-dictating what peer support should look like,” says Allison Dunning of Peer Support Canada. “Part of the value of peer support is the authenticity and humanness that it brings to the system.”

A rush to standardization could also aggravate a lack of diversity in mental health care. Viewing all people with lived experience, and by extension peer supporters with lived experience, as having the same needs and interests can perpetuate harm already present within the sector. In a 2016 Philosophy, Psychiatry, & Psychology article, Jijian Voronka, an author and associate professor at the University of Windsor, Ont., noted that people with lived experience who were able to work in the mental health system were “by and large ones recognized as able to perform White civility, comprehensibility, and self-manage unruliness.”
This bias was felt by the authors of the Mad People of Colour manifesto. Published in Asylum magazine in 2013 by a group of racialized mental health activists, the manifesto described how racialized people are dismissed or deflected in mental health advocacy: “The mad movement presents a mad identity based on white people’s experiences and white people’s theories. Tell us, is madness something that only white people experience?”
According to the Mental Health Commission of Canada, primarily white, middle-aged and urban mental health consumers have been the face of the peer support movement. That’s why, Dunning explains, peer supporters, and the sector in general, have to pay more attention to factors like race and culture. “For example, I’m a white, cisgender, female settler who has navigated our mental health system with a certain diagnosis,” she says. “I can support someone with the same diagnosis, but that doesn’t necessarily mean I can fully empathize with their experience because of the context they might come from. If they’re a Black person navigating the system, [they’re going to have a different experience] than me.”
Bellamy, who is Black, says her sister encountered this barrier when seeking therapy. “My sister — she’s a powerhouse, and she also speaks a lot of slang. Years ago, when she went to therapy, she had to translate everything. Everything she said she had to translate to the therapist.” Bellamy believes peer supporters from underrepresented communities can be really helpful because they can connect through shared lived experience.
Canada’s mental health system was stretched to its seams before the pandemic started, and soaring mental health needs are only further fraying its threads. Peer support could help ease the stress and fill gaps in the system, but it’s simply not being used as much as it could be. “We don’t have enough financial support to be able to have peer support exist as much as people would benefit from it existing, which is unfortunate,” says Dunning. “The wait times, the system’s capacity to support people with mental health challenges is just inadequate. We need all the help we can get.”
So given the economic, personal and practical benefits of peer support, why isn’t the government doing more to fund it at a time of increased need?
”If we’re really going to talk about peer support as its own discipline and its own field, there should be career opportunities. There should be that next step available for peer support workers to see a path for themselves.”
Paige Lougheed, provincial peer support co-ordinator for Foundry
“Sometimes, peer support is seen as this thing on the side…so there’s not necessarily a lot invested into it,” says Asante Haughton, peer development and training manager at Stella’s Place in Toronto. “More buy-in [from the mental health sector] will support us in creating more programs, and better programs.”
A bolstered peer support system in Canada could ease the systemic barriers involved in receiving help for mental illness, but standardization has its pitfalls. Professionalizing the peer support space would mean more job security for its workers, less burnout and a stronger continuum of care for those receiving peer support, but it needs to be done carefully and inclusively so as not to damage the human connection at the heart of peer support.
“The conversation has been around peer support versus other things when, in reality, the conversation should be peer support plus other things,” Haughton says. “Then everyone is at the table providing the value of whatever discipline they’re in — it’s just adding more spice to the mix. You’re turning a bland recipe into something really delicious.”
For Susana Meza, the importance of her work sharpened into focus at the beginning of the pandemic. At the time, she was doing peer support work at George Brown College, adapting a drop-in peer support program to a virtual space. She trained through various Toronto organizations to ensure the space was as supportive as possible. The program grew into a tight-knit community where its participants could make art, unwind and talk during a bleak and confusing time filled with uncertainty. After the program wrapped, one of its participants kept creating, which led to Meza curating her participant’s first art exhibit in 2022.
“We are all really in this together — in our fears, in our dread of life, in our love of life, in all the chaos that happens in the mind and the heart, and peer support really brought that into the spotlight for me,” Meza says. “It helps me stay, as I say, ‘on the yellow brick road,’ away from my drug of choice because being there for each other definitely works. It’s the simplest thing, but it’s so powerful.”
***
Miranda Newman is a writer and editor in Toronto.
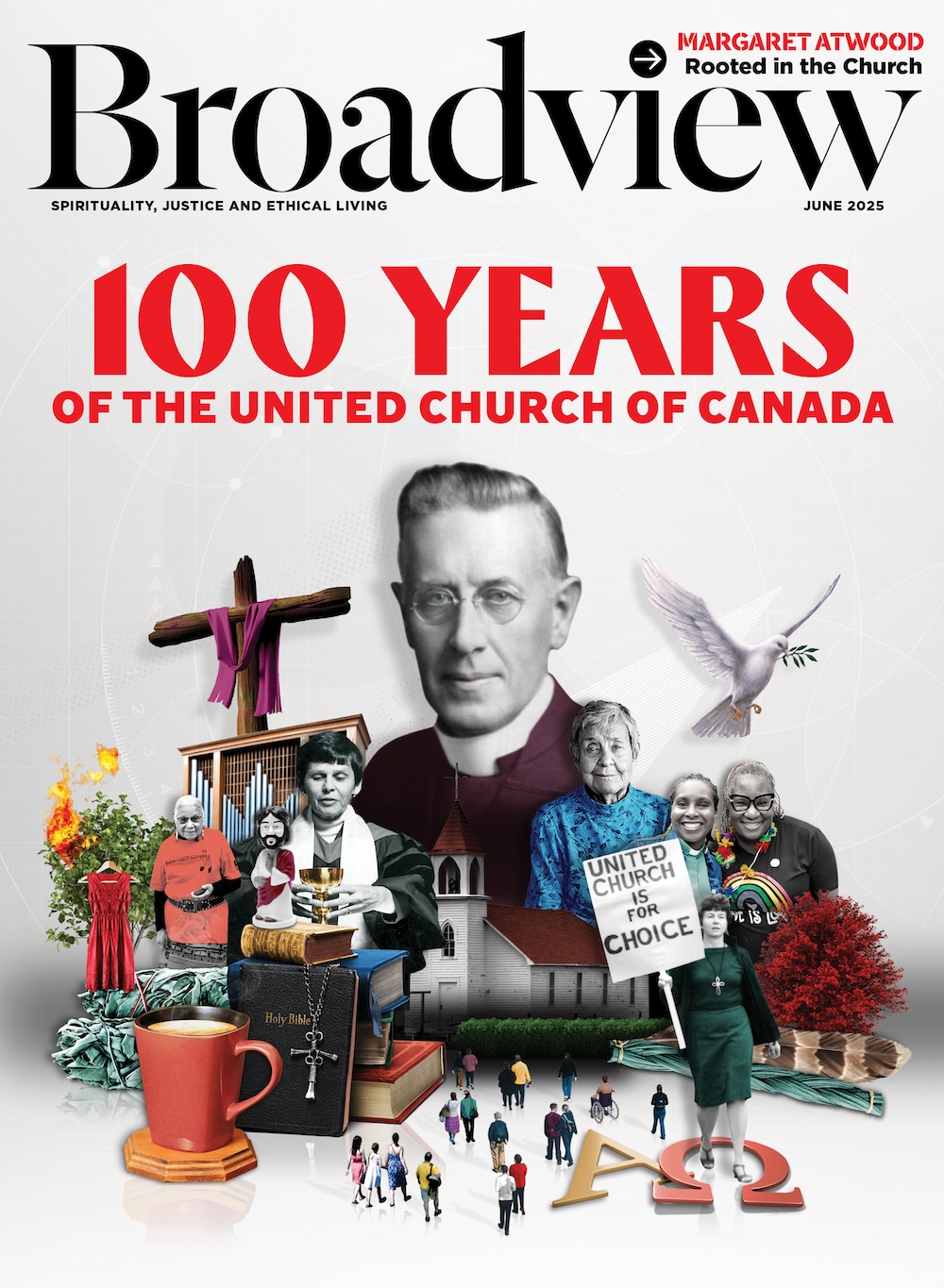
This story first appeared in Broadview’s October/November 2022 issue with the title “Heart and soul.”














It’s encouraging to hear that peer support workers are being considered as a potential solution to address Canada’s increasing mental health needs. Peer support workers can bring a unique perspective and understanding to those who are struggling with mental health issues, as they may have had similar experiences themselves. By providing support and guidance, peer support workers can help individuals on their path to recovery and improve overall mental health outcomes. It’s important to continue exploring and investing in different approaches to mental health care in order to meet the growing demand for these services.