Katie Leahy, a registered nurse, arrives for the patient’s checkup by bicycle, wearing a black rain jacket and thick-soled boots for the drizzly weather that’s typical in early spring on Vancouver Island.
Dr. Fraser Black, having parked his scooter around the corner, meets Leahy at the entrance of an apartment building on the edge of downtown Victoria. Before meeting with their patient, who’s staying with a close friend, they discuss her blood work results and how her health has changed from the week prior.
Leahy and Black are part of Victoria’s Palliative Outreach Resource Team (PORT). It’s a mobile service that brings medical care directly to people who are homeless and living in poverty with serious, often terminal, illnesses. PORT can also connect clients to specialized health services, mental health supports, faith leaders and more.
Their patient, Ille Jocelyn, is dying. She’s barely over 50 years old. When she first went to hospital with cancer in 2016, she’d fallen on hard times. She was going through a messy divorce and didn’t have stable housing or a support network. Her cancer left her in unbearable pain, and without consistent health care, she was in and out of hospital emergency departments. She spent time sleeping on the streets in downtown Victoria. In 2019, a social worker introduced Jocelyn to Leahy and Black, who both specialize in palliative care.
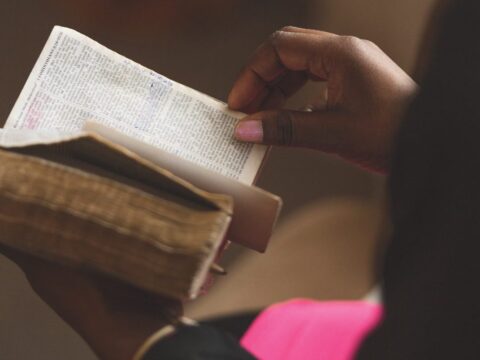
Palliative care is a medical approach that emerged in Canada in the mid-1970s. It doesn’t speed up or delay death. Rather, it acknowledges death as a normal part of life. Patients with serious diseases develop “severe physical, psychosocial, and spiritual symptoms before death,” according to a report published in the Journal of Palliative Medicine, and “there is strong evidence that [palliative care] is beneficial in reducing much of this suffering in patients, as well as psychosocial and spiritual or existential distress in families.” Simply, palliative care improves the quality of life for the dying individual and those around them.
In Canada, estimates for the average life expectancy of people who are homeless or vulnerably housed are as low as 39 to 59 years old, significantly shorter than the national average of 82. That’s because living in poverty has chronic negative health effects, as these people are less likely to have access to resources that can improve their health, such as housing, nutritious food, job security and consistent medical care.
Additionally, those living with substance use challenges, mental illness, and colonial and institutional traumas are more likely to face barriers when trying to access social services and basic resources. Up to 67 percent of homeless individuals report having a mental illness, and having a mental illness makes them twice as likely to depend on drugs and alcohol. As such, people with serious illnesses in this population are often diagnosed late, when little can be done to treat their disease.
Current models of palliative care, for the most part, are not designed to serve Canadians who face inadequate housing, racialization or stigmatization because of substance use and mental illness, according to a 2017 article published in the Canadian journal Current Oncology. The piece states: “For those people, death and dying…are more likely to occur in acute care [such as ambulances or emergency rooms]. Or people die alone, outdoors, on the street and in vehicles, or in shelters or transitional housing, cared for by workers who are highly compassionate, but who have limited training and knowledge to ensure quality end-of-life care.”
Further, a 2019 report in the journal Progress in Palliative Care reveals that Canada’s palliative care system tends to serve a more privileged patient: one who is usually white, has a strong social network and family ties, and has the financial means to pay for supplementary care in their own home.
Most of us, when we imagine the ends of our lives, likely assume there will be a comfortable bed. We hope to be surrounded by those who love and care for us. We take it for granted that we will have food while we can still eat and will access pain medication as needed. Could a good death also be within reach for Canadians who are homeless?
Eahy and Black climb three flights of stairs. They knock on an apartment door, and Jocelyn’s friend Patrick Smith welcomes them inside his home. Jocelyn sits upright in the bed, just steps from the front door. Bottles of pills, prescribed by Black, balance on the headboard, and a walker stands at the bed’s base. Her lime-green T-shirt peeks out from the handmade quilt that rests on top of her, warming her thin body.
After exchanging a few jokes, Black and Leahy get to work. They talk about adjusting Jocelyn’s medications. They ask her how she’s feeling, how she’s managing, and what’s new with her health and in her life. They listen, unhurried.
She’s tired, she says. She’s never free of pain, but it has been manageable recently. She can even move around a little.
“May I?” asks Black. Jocelyn nods, and he lifts the quilt to examine her swollen foot. After recapping the next steps in her care, Leahy and Black ask Jocelyn if she still has phone minutes available to make a call if there’s an emergency. They give her a gift card to help with groceries. Then, they leave to check on their next patient, located elsewhere in Victoria’s inner city.
More on Broadview:
- United Church national body updates MAID stance
- How my husband and I spent our final hours together
- Most Canadians want more control over end-of-life choices: survey
For Jocelyn, this compassionate care is entirely different from when she was first hospitalized in 2016. She felt stigmatized by many of the doctors.
“Every time I went back [to the hospital], they’d always ask if I’d been out using drugs,” says Jocelyn. And when they prescribed painkillers, “I was getting such tiny amounts that it wasn’t helping.” Mostly, she felt like she couldn’t trust the health-care system to offer her the care she needed.
Leahy and Black are not the first health-care professionals in Canada to provide palliative care for the homeless. Three decades ago, Dr. Susan Burgess began offering such help when she moved to Vancouver in 1993. At the time, the city was in the midst of its second AIDS epidemic, and the epicentre was in the Downtown Eastside, among injection drug users, many of whom were living in poverty.
Burgess, a palliative care physician, saw how traditional medical clinics were unable to tackle what was happening. Her patients were resilient, persevering to find a bed for the night or a meal for the day, but medical appointments in a brick-and-mortar location were not a priority.
“These patients aren’t organized the way the medical system expects them to be: to make an appointment, keep an appointment, delay gratification to go, and then to be told that they smoke too much and shouldn’t use drugs,” says Burgess. That meant not getting diagnoses, treatment or medication. It meant death, often in extreme pain, alone or removed from their community.
“People were just dropping like flies,” says Burgess. “It was an obvious question for me personally: where are people when they’re sick and dying and can’t get help? Well, they’re on the street [and] in shelters. They don’t have family. They self-medicate quite effectively. However, it’s so effective that when they are near death, they get transported to the emergency department and die there.”
Nothing about that end-of-life experience sat right with Burgess. She saw a need to do better for these patients, ensuring they weren’t marginalized in death as they were in life. During this epidemic, Vancouver Native Health — the service provider where Burgess worked at the time — had started HIV outreach programs, bringing care directly to the city’s homeless population. Outreach and shelter workers recognized when patients they saw regularly began to look ill and connected them to existing health-care services. But they were missing an important element: patients needed a doctor to bring prescriptions directly to them.
“Not only did you have chronically ill people who were already in poverty here, but now, overlying that, were people with severe mental illnesses who were becoming infected with HIV. Going to a clinic was not going to happen for them,” says Burgess. “We decided that most of what we were doing could actually happen where people were, if we were respectful in entering their space.”
Today, Burgess quietly continues to bring end-of-life care directly to the homeless population in Vancouver’s Downtown Eastside. In the decades since she began this work, physicians in other parts of the country noticed that their city’s vulnerable were also falling through the cracks at life’s end. In 2001, the Diane Morrison Hospice opened in Ottawa, providing palliative care to homeless and street-involved individuals. In 2014, Dr. Naheed Dosani launched Palliative Education and Care for the Homeless (PEACH) at Inner City Health Associates in Toronto. And in 2016, Dr. Simon Colgan and Rachael Edwards, a registered nurse, launched the Calgary Allied Mobile Palliative Program (CAMPP).
Change is happening, but these models are still the exception, not the norm. They all differ slightly in how they’re run and funded, and none reach a rural homeless community. Widespread, national change is still needed to cohesively address the issue. And that can’t happen without evidence backing the success of mobile palliative care models.
Compiling that proof is exactly what Kelli Stajduhar is doing. Stajduhar is a professor in the School of Nursing at the University of Victoria and a research affiliate in the university’s Institute on Aging and Lifelong Health. She is also a palliative care nurse with more than three decades of experience. In 2014, Stajduhar began a study examining the end-of-life experience for homeless and vulnerable individuals in Victoria. This research, published in the report “Too Little, Too Late: How We Fail Vulnerable Canadians as They Die and What to Do About It,” is the base around which PORT was built and a key reason for its launch in 2019.
Over a two-year period, Stajduhar’s research team interviewed and observed 25 people with terminal conditions living in Victoria’s inner city. Service providers, including nurses, support workers and housing workers, were interviewed, too. The team spent over 300 hours observing the patients’ experiences, seeing how they moved through the health-care system — and how they fell through the system’s gaps.
The findings were published in the peer-reviewed medical journal BMC Palliative Care in 2019. Barriers to accessing palliative care include the normalization of death in the street community, where overdoses are common. It can be challenging for workers without medical training to identify who needs palliative care. Health authorities might deem patients’ places of living unsafe for care providers to visit. And it’s difficult and confusing to try to navigate the healthcare system, especially without access to transportation, money, a cellphone or a support team.
“We are all human, we are all fragile and we all face mortality.…The challenge is that we have undignified structures that make it very challenging for certain people.”
Kevin Rodrigues
Bringing palliative care directly to those who need it removes some barriers. During the study, 13 of the 25 subjects died. Most received palliative care and accessed services they didn’t think were available to them.
“A client we interviewed said, ‘Since I got cancer, it’s been nothing but good for me,’” says Stajduhar, describing how palliative care helped the study subjects. “For the first time in their life, somebody believed they had pain. Options for housing became available. People in the health-care system were treating them well because we were doing all kinds of advocacy. Everything becomes easier.”
Tony’s* entire life was in his car. Every day or so, he moved it to a new spot in Victoria to avoid getting towed. If that happened, there was no way he would be able to pay to get his car back — to get his home back. That’s how Tony was living when Leahy and Black began offering him palliative care for his cancer. As his health deteriorated, Leahy and Black spoke with Tony about his wishes. Did he want to move into a hospice? Or try chemotherapy? Was fighting for more time important to him? No, he said. He didn’t want any of that. He just wanted to be as pain-free as possible as the cancer took its course. He wanted to find a way to reconnect with his family. For Tony, palliative care meant staying in an environment he knew for as long as possible. It meant pain management. When a serious infection required Tony to be hospitalized, he said goodbye to his family — the PORT team had found them. They were at his bedside as he died.
“A good death for this population means giving space for people to live the life that they’ve been living without judgment,” says Leahy. “It’s meeting the person where they are at and letting them be the person that they need to be…and then still showing up, time after time. It’s giving them choices and honouring their choices.”
The alternative is traumatizing, both to experience and to witness. Leahy tells stories of vulnerable people who don’t have access to palliative care. Many die alone, with no food, no phone and no one to call for help. Sometimes they’re only found days later.
According to Leahy, an integral part of providing palliative care to her PORT clients is building trust. “In the general population, trust is assumed with a health-care provider. And that is a privilege,” she says, adding that traditional health-care settings can awaken traumas or not feel like safe, judgment-free places. That’s why Leahy and Black take time getting to know their patients and their stories. Once that connection is forged, clients are more likely to open up and share their wishes. And Leahy says those wishes are often similar. Her patients want a phone with prepaid minutes so they can call her for help in an emergency. They want food. They want a bed.
For some, a good death also prioritizes religious beliefs, and offering spiritual counsel is another element of PORT’s care. The team works to understand if clients practise a faith — whether they might turn to a priest, rabbi or Elder in times of struggle — and where they find hope
“It’s not uncommon when people are coming to the end of their life…to seek out some conversation about the meaning of life,” says Stajduhar. “Some people want to make amends with whatever god they might believe in.”
The PORT team hasn’t yet had requests for overtly religious counsel like prayer or last rites. But they’re able to refer clients to a religious leader if requested. “Our work is so dependent on the relationships that we build with people,” says Stajduhar. “There are ministers and priests in town that have experience working with this community, so if there was a call for it, we would reach out to them.”
Kevin Rodrigues, formerly a chaplain at St. Michael’s Hospital in Toronto, has direct experience providing spiritual care to homeless palliative patients. For him, those interactions were often about modelling religious values of acceptance and community. These days, Rodrigues works as a bioethicist at Toronto’s University Health Network, educating clinicians and offering ethics consultations in-clinic. He focuses on how factors like housing, socioeconomic status, race and gender affect equitable access to health care.
Rodrigues believes that palliative care should be available to all. “Society is judged by how they treat their most vulnerable people,” he says. If we ask who the most vulnerable people are in our society and align our moral compass to that, it might lead to different kinds of policy decisions. “Why would people be denied a good death simply because of where they stand in our society?” he questions.
On the other hand, as some might argue, doesn’t the drug user choose that lifestyle? Couldn’t the individual with cancer have sought help before their tumour became a fungating wound? Isn’t it true that the person with schizophrenia who runs away from hospital doesn’t want to be helped?
When it comes to free will, Rodrigues says that “some people are making choices that are informed by a lack of actual choices,” while those who have privilege “may have an abundance of other choices to make. Even if we were to say people make [their own] choices, are these choices truly free when they are embedded in an unjust system?”
Rodrigues adds that it’s important to consider how health care can best be delivered to patients with a history of trauma, those with reduced decision-making capacity and those from disadvantaged backgrounds.
“We are all human, we are all fragile and we all face mortality.…The challenge is that we have undignified structures that make it very challenging for certain people,” he says. “Those of us that have privilege and that have access to structures of power have to find ways to apply that to level the playing field and find opportunity for others to achieve, really, what’s a basic human right: a dignified life, a dignified death.”
Ille Jocelyn knew in early spring that her cancer was incurable. And just as the days began to get longer and warmer last May, she died. She didn’t die alone or in a dark downtown alley. She didn’t die delirious from pain. She died in a bed, cared for by people she trusted, with her end-of-life wishes fulfilled.
At the time of her death, a shroud of uncertainty hung over the world, burying it under the weight of the COVID-19 pandemic. Despite his heavy grief, Jocelyn’s friend Patrick Smith held a socially distanced memorial shortly after her passing.
A small group gathered in May. Together, they grieved. Together, they shared memories of Jocelyn. They talked about her quick sense of humour and her fierce intelligence. They shared stories from when she owned a chocolate factory and helped lead a hedgehog rescue society.
And years after that springtime gathering, that group of people will remember who Ille Jocelyn was, beyond the challenges she experienced in life.
It’s what everyone deserves.
*Name has been changed
This story first appeared in Broadview’s December 2020 issue with the title “Who deserves a good death?”
Karin Olafson is a freelance writer in Vancouver.
We hope you found this Broadview article engaging.
Our team is working hard to bring you more independent, award-winning journalism. But Broadview is a nonprofit and these are tough times for magazines. Please consider supporting our work. There are a number of ways to do so:
- Subscribe to our magazine and you’ll receive intelligent, timely stories and perspectives delivered to your home 10 times a year.
- Donate to our Friends Fund.
- Give the gift of Broadview to someone special in your life and make a difference!
Thank you for being such wonderful readers.
Jocelyn Bell
Editor/Publisher