Since I am 72 years old, I am designated as “high-risk” in this COVID-19 crisis, even without underlying disease conditions. Prior to the pandemic, I had come across a line in a book on aging: “I am old enough to die.” It felt true. When I say that to people, and in the present context add “and I don’t want a ventilator,” gasps are heard at the other end of the phone line. I have stopped saying it.
I spent years as a palliative care nurse in both home and hospital settings, and later as a chaplain to patients who were dying but were not taken to the intensive care unit. My experiences convinced me that a non-ICU death was a more humane way to die.
When I walked the corridors of the active teaching hospital during my tenure as chaplain (now called a spiritual care provider) in the 1980s and ‘90s, I came to understand that death was not the worst thing that could happen to us. This growing sentiment led to doctoral research and a thesis about the experiences of doctors and nurses with dying patients in intensive care units. I observed that the medical treatment received in an ICU during the final stages of life, and of death, appeared to give little comfort to patients and in fact, most often prolonged their suffering. One participant, a research physician, observed: “non-beneficial treatment continues because ‘It’s just automatic… no thought’s given to it…because you get swept up into it.’” An intern stated, “You do everything…because you went into medicine to do everything.”
It helps to become more comfortable with grief.
In the time of COVID-19, dying in hospital is fraught. A front-line spiritual care provider describes her experience with dying COVID-19 patients as such: following the process of putting on three gowns, and all the necessary hand, head and face gear, her own heated discomfort fades as she connects — by way of iPhone — with the patient’s family, who cannot enter the hospital. She invites each one to say goodbye. They do. The patient can hear but not always respond.
“Is anyone with the patients when they actually die?” I ask.
“Not always,” I’m told.
This breaks my heart. My visceral experience of being at the bedside of a dying person with their family — the holding of hands, moments of prayer or singing, when wanted — peace is palpable when all are accepting the reality of pending death. It is a holy experience. Often there are no words, simply a fulsome silence. The physical contact, the ability to cry with others, the rituals – they are all part of the healing.
More on Broadview: During COVID-19, I find freedom in a slower pace
Part of preparation for our own death is to understand what treatment is appropriate, if we have a disease that is progressing. My research showed that physicians feel satisfaction and excitement bringing people back from the “brink of death.” At the same time, both ICU nurses and doctors agreed that extreme treatment occurs in the ICU, fuelled often by unrealistic expectations on the part of families. In her book That Good Night: Life and Medicine in the Eleventh Hour, Dr. Sunita Puri describes the “tension between medicine’s impulse to preserve life at all costs and [the] spiritual embrace of life’s temporality.” We all need to become more comfortable with death, when death is what is happening.
It helps to become more comfortable with grief. When we are dying, we lose everything and everybody that is important to us. When we give ourselves permission to feel the full weight of the feelings associated with any of our losses, and the many small losses of our recent COVID-19 experience might benefit us here, we prepare for the big one – our own death. We can begin to learn to live with loss in a way that helps us and others accept that dying is not the worst thing that can happen.
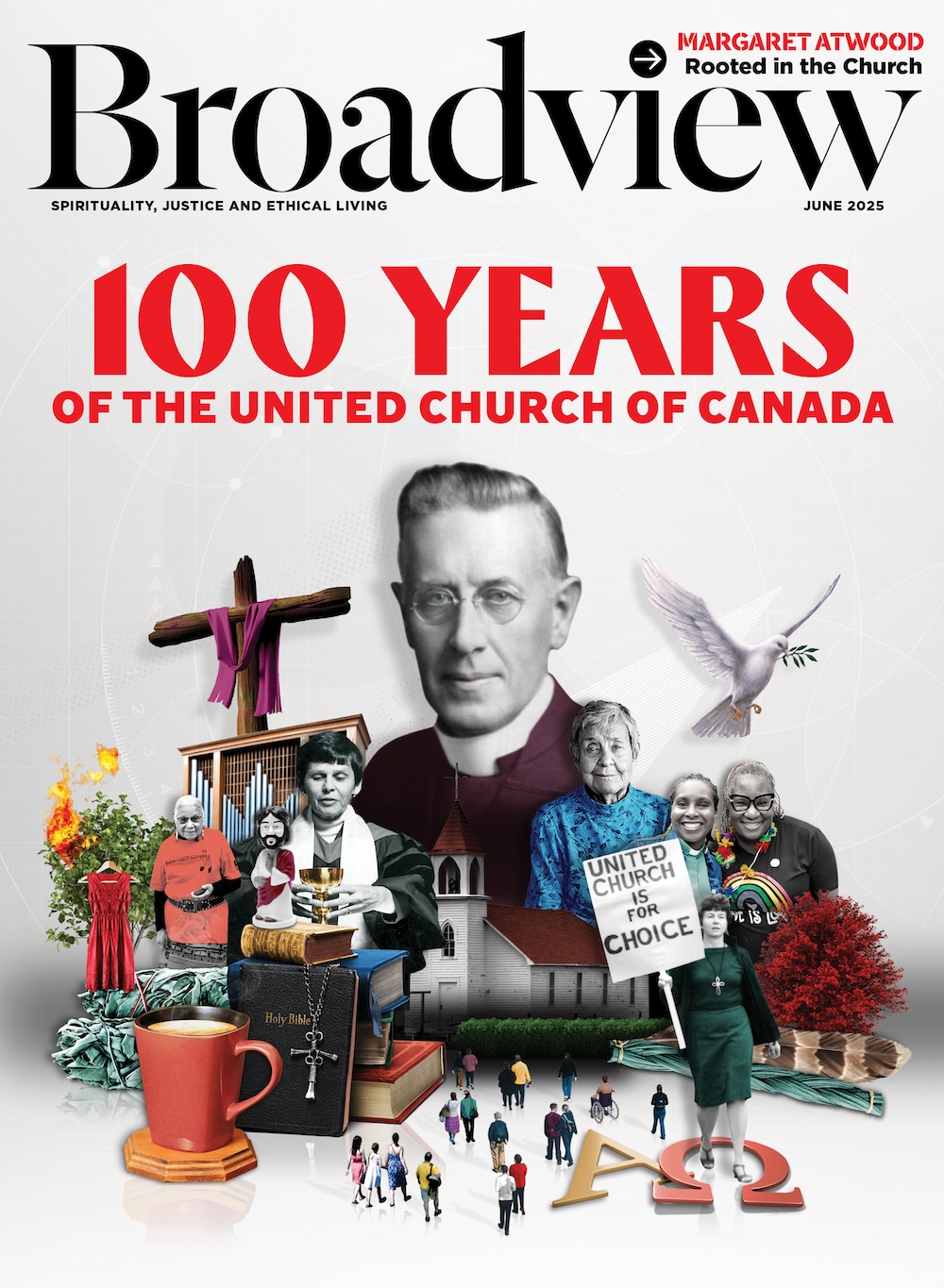
Broadview is an award-winning progressive Christian magazine, featuring stories about spirituality, justice and ethical living. For more of our content, subscribe to the magazine today.














This is a helpful article. I told my family weeks ago that if I become critically ill with COVID 19 I do not want to be intubated, a necessary part of ventilator treatment. When I told my Dr. the same (during a recent phone call when she impressed upon me how vulnerable I am if I become infected), there was silence on her end. Anne Simmonds does a great job here of describing why I made this decision and how it’s often difficult for others to hear. I’ve learned that by accepting my mortality more completely, I am living more fully.
Thanks for this reflection, Mardi. Very helpful.Blessings to you folks.
Having been intubated during jaw surgery, I know how uncomfortable it is. After the critical period, it was also uncomfortable being suctioned to prevent pneumonia while “recuperating”. I guess the conclusion is I’m still here because of it. I also volunteered and worked in palliative care and came to the conclusion “I wouldn’t want to go through that any longer than I did.” (1 month, let alone a “lifetime”)
We have so improved our ability to enhance and prolong life, that we now have more ethical questions rather than answers.
God created us to live eternally, and we ruined that chance through sin. Funny, apart from God, man still has that “hope” that one day we can reach that point of living forever, making ourselves as God.
Thanks for this, Anne. It brought to mind similar times for me during my CPE training in a teaching hospital south of Philadelphia. This was during the Vietnam War. One day I was called to the bedside of a woman experiencing her final moments. The family surrounded her were sad, but serene, and welcomed me as I arrived. Gentle explanations of their loved ones’ situation were shared, and I was asked to offer a prayer. As we surrounded her, holding hands, with a nurse included in our circle, a young doctor rushed in, moved family members aside, and proceeded to do extraordinary measures to “save” the patient! You can imagine the horror of the rest of us. Later, after the patient had died and the doctor and family had left the room, I caught up with this young physician. He was quite sober, after seeing how his abrupt intervention had been so devastating. And then he explained to me he had served in Vietnam, on the battlefield, where instinctively. quick, aggressive measures were commonplace as medics raced to care for the gravely wounded… to do whatever it took to save them right on the spot. Even fairly extreme measures. All I can add was that an in-person conversation I arranged later with the doctor and members of the deceased’s family was a time of profound grace for us all, thanks largely to the forgiving family who, in their own grief, recognized and embraced what was, I believe, someone Henri Nouwen would have accepted as “a wounded healer.”