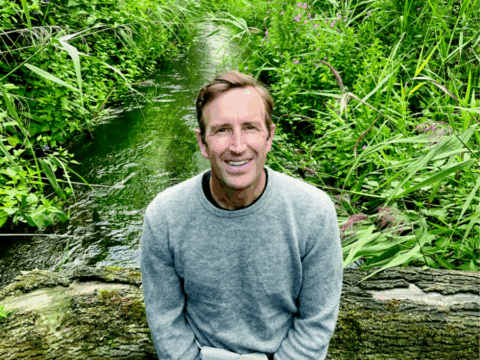
Mark Paci is a spiritual care practitioner at St. Michael’s Hospital in downtown Toronto. His day-to-day routines have changed drastically since the onset of COVID-19. Kate Spencer spoke to him to find out what life is like for a hospital chaplain during a global pandemic.
Kate Spencer: What are you wearing to work these days?
Mark Paci: I usually wear my own clothes, but anyone having contact with patients is wearing scrubs now. Then we’re given two regular surgical masks each day that we wear at all times. As a chaplain you would never go into a COVID patient’s room; you would call in because you’re not absolutely essential. But even with a presumed COVID patient, you put on a gown, you put on a visor, and you put on gloves.
KS: How does that change the way you interact with people?
MP: It’s really strange because there are all these layers between you and the person who’s vulnerable. It’s very impersonal, very “I’m healthy, you’re sick.” As a chaplain, communication is about behaviour and body language, and if they can’t see you smile, it’s harder.

KS: How do you work around that barrier?
MP: I notice myself using my body more, using my hands to speak, using my voice. I’m speaking louder and enunciating more. And then, oddly, using my eyes. I’m aware of what my eyes are saying, I suppose, more than usual. You become more anonymous. People don’t know who you are. I find I have to define what I do more.
KS: Tell me about the general environment of the hospital. How do things feel?
MP: Obviously the ICU and Emergency… it’s tense. People are very, very cautious of what they’re wearing, how they’re putting on their stuff and taking it off. There’s a lot of humour in the hospital among staff, and there still is generally, but there’s a clear absence of it around COVID.
KS: How are patients coping?
MP: One of my units is inpatient psychiatry, and my experience during COVID is that fear and anxiety are amplified with those who suffer from mental illness, as well as loneliness. The imposed isolation augments the isolation experienced by those who struggle with mental illness.
KS: What is it like to work with people who have tested positive for COVID?
MP: I honestly haven’t done that yet. I’ve heard from colleagues that it’s very difficult. Some people can’t even speak. So not only are they removed physically, but they can’t respond. You’re almost speaking into a void, and you’re hoping something reaches, something lands, that you’re offering some form of comfort.
More on Broadview: COVID-19 testing is vital. Here’s what we need.
KS: How are the families?
MP: Families will come in, and some are assuming that they can go up to the unit and see their loved one, but they can’t. There are no visitors whatsoever, with one exception; if a patient is imminently dying, they get one visitor. I can only imagine what it would be like if my wife was in the ICU and I couldn’t see her — it would just be overwhelming anger and frustration and sadness. I met with one woman who was just trying to bargain, just trying to find the right words to get up to the unit. It took her a very long time to accept the fact that she couldn’t.
KS: What tactics do you find yourself using to offer comfort to COVID-related patients and families?
MP: Often there aren’t words you can offer someone that’s in a state of that kind of grief and fear. It’s always about presence, but especially during COVID, no one really knows how to do this. People are discovering it as they go, in a very real way. The training that I’ve gotten has prepared me for being able to hold the space of whatever is going on. So if it’s anger, or sadness, or fear, or whatever it is, to allow that to happen, and to not turn away from it.
As a chaplain, communication is about behaviour and body language, and if they can’t see you smile, it’s harder.
KS: Is there anything that’s shifted in the way you work with people that you would like to bring into your future work?
MP: I don’t want to sound sentimental, but the connection between people, the closeness between people, our ability to be vulnerable with each other. I think the assumption, especially in the medical world, is that we’re in control, and if you have a disease we’re going to fix you. I think this is really showing we’re not in full control. What’s important is coming to the fore, which is how we take care of each other and how we take care of the vulnerable.
This interview has been edited for length and clarity.
Broadview is an award-winning progressive Christian magazine, featuring stories about spirituality, justice and ethical living. For more of our content, subscribe to the magazine today.











Thanks for publishing succinctly, yet in heart-felt ways what such pandemic serving experience has taught a person about what’s really important about how we relate to each other!