Jyan Nath checked her husband, Gyan, into the hospital with chest pain, thinking she’d have him home soon. Two days later, he was in a coma. The coma was brought on by septic shock, leaving him on life support for nine days, which ultimately resulted in brain damage. Always an active man — he and Jyan loved to travel and did community volunteer work — he had to move into a long-term care facility after six months in the hospital. “That was very hard because these homes are not culturally sensitive — the language is different, the treatment is different,” says Jyan. The couple, of Indian descent, came to Canada from Fiji in 1962, part of a wave of immigration fulfilling a shortage of teachers. They arrived in Nelson, B.C., eventually settling in Vancouver, where Jyan was a special education teacher at the elementary level while Gyan taught business to high school students.
Jyan visited her husband in the morning and evening while he was in the care home. She hired a support worker to come daily at lunchtime so she could get a break. She and Gyan were vegetarian, and the options at the facility, like mashed potatoes and boiled peas, left much to be desired. She brought food every day, mostly staples Gyan was used to: rice and daal, curries, yogurt and roti.
You may unsubscribe from any of our newsletters at any time.
While they had planned well financially for their future and were able to manage the expenses, the facility ultimately didn’t fulfil Gyan’s needs. They paid $3,000 a month in fees for the home, and yet Jyan was still providing food every day and paying an additional $1,000 for the caregiver. It opened Jyan’s eyes to the gaps in care that people like her husband were experiencing.
Gyan died in the care home almost a decade ago. Jyan Nath is active and independent at 88, but for the last few years she has been looking for care options that cater to her lifestyle — partially informed by her culture and religion. Unfortunately, the landscape hasn’t changed much.

A fifth of Canadians are foreign-born, and as the population ages, there’s an increasing need for culturally competent long-term care (LTC) that would suit the needs of someone like Nath. Language and religious identity are just two reasons why culturally competent care matters. Research shows that everyday comforts, like eating familiar food, can greatly impact a senior’s quality of life in an LTC home. The Wellesley Institute, a Toronto-based health policy think-tank, noted that “linguistic and ethno-specific care services have positive impacts on residents’ physical and mental health such as reduced isolation, lower rates of depression, and fewer falls and hospitalizations.”
While this kind of care exists in Canada, access across the country is uneven. No national database exists to help families find suitable places. And wait times, which can be up to nine years for mainstream LTC homes, are often even longer for culturally specific facilities. In the absence of truly accessible options, immigrant families are making tough choices about care.
More on Broadview:
- For-profit long-term care fails residents and workers. The solution is clear.
- Faith leaders call on Ontario to fix long-term care system
- Mobile palliative care services bring comfort to Canada’s most vulnerable
Seong-gee Um, a senior researcher at the Wellesley Institute, has been examining this issue for the past six years. It has been a much-discussed topic in the Korean Canadian community, and she realized other cultures were facing the same challenges. And while she found many documents by Canadian researchers and policy-makers that touch on equity or diversity, none of them offered strategies, initiatives or solutions.
Any mainstream movement on culturally competent care has stalled, she says. Seniors are suffering, and in some cases dying, before they can get a long-term care bed in an ethno-specific home. Meanwhile family members, particularly women, are bearing the brunt of caregiving.
One of the reasons these seniors aren’t heard in the policy discussions about long-term care is language barriers. Um is hoping to change that. In a January paper she co-authored, participants in the Greater Toronto Area from regions including Italy, South Asia, the Caribbean and China were interviewed in their own language about decision-making for elderly immigrants.
Even when there is support at home, like a personal care worker, says Um, if the senior doesn’t speak English or French, it adds another layer of caregiving for someone to act as an interpreter. In many households, that means there’s no real break. Um and her co-authors found that just over half of family caregivers spend more than 40 hours a week assisting older adults with tasks like cooking or taking medication, and accompanying them to appointments. The emotional impact extends to the rest of the family as one member is tied up with caregiving. And there can also be financial implications as people quit their jobs or reduce their hours to take on more care responsibilities.
Before Christelle Saint-Julien takes a job, she’s upfront that she needs flexibility to care for her 81-year-old father, Pierre-Bolté. The Montreal journalist moves between freelance and full-time contracts, giving her the time she needs to help her younger brother, who lives with their father. She visits multiple times a week and spends one day over the weekend helping out with bathing, dressing and cooking.
“A more traditional work schedule wouldn’t allow me to do that,” says Saint-Julien. And she sees how tough it is for her brother, who works a much more rigid job in finance. In a strange twist, the pandemic has meant they have been able to keep their father at home longer, since her brother isn’t going to his office. But they can’t keep that up and have recently put him on a list for a nearby long-term care home. “Now he’s at a point where he is forgetting names,” she says.
Pierre-Bolté came to Montreal from Haiti in the 1970s and worked as a taxi driver into his 70s. He loved driving, so working wasn’t an issue for him, until he started to forget where he was going in a city he knew intimately. He was diagnosed with Alzheimer’s. At first, the progression of the disease was slow, but now he needs constant care. Much to Saint-Julien’s surprise, the options for publicly funded at-home care were limited, although she’s grateful to have a support worker help her father dress every morning.
In the absence of truly accessible options, immigrant families are making tough choices about care.
In the public system, she and her brother don’t have the choice of culturally specific care homes, and they don’t have the financial means to pursue private centres. She’s noticed many support staff at facilities are Black or people of colour, which makes her feel better, and the case worker they have been consulting with is very conscious of these issues. But given the uncertainty around the pandemic and its ongoing impact on long-term care homes, they are cautious about whether to place their father in a facility when a bed becomes available.
Part of the reason they have kept him at home as long as they have is cultural, says Saint-Julien, which surprised her since both she and her brother are born and raised in Canada. Research shows this sense of filial duty is common across many cultures, with adult children feeling a strong obligation to care for parents at home and share the responsibilities among siblings.
Another reason Saint-Julien has opted to care for Pierre-Bolté is simple: “He’s such a great dad.” He was an extrovert who loved visiting friends. And now that he isn’t able to, she’s invested in ensuring he has the best quality of life possible. She calls him several times a day to give him something to do, even though she knows he won’t remember what they talked about. When she goes over, they hang out and watch television or she reads aloud to him.

His longing for familiar things has also influenced their decision to keep him at home as long as they can. As his Alzheimer’s progresses, he’s become more attached to eating Haitian food. He seems less comfortable “having people around him that don’t look like him,” says Saint-Julien, who adds this was never an issue before. He’s also slowly losing language; he’s forgotten English, and while he will still respond to French, he will often speak in his first language, Haitian Creole.
This harkening back to childhood touchstones is common in immigrant seniors even if they aren’t experiencing memory loss, says Karen Kobayashi, a social gerontologist who is an associate dean in the faculty of social sciences at the University of Victoria. It is related to changes in the brain as we age, she says. People often want to visit their home country and look for ways to reconnect through language or culture. “We want to continue to have a connection to our roots,” says Kobayashi.
And it’s not only important to first-generation immigrants. Kobayashi uses the example of her father, who is second-generation Japanese Canadian and is on the list for Momiji, a Japanese supportive living facility in Ontario. Her father’s generation experienced internment camps, and despite being raised in Canada, “there’s still a pull towards what we would call a culturally sensitive understanding of norms, values and beliefs of a particular cultural community that is somewhat at odds with western Canadian culture,” she explains.
Culturally competent care means being able to speak the language you are more comfortable with and eating familiar food. It is also about cultural sensibilities. It can be something as small as a care worker asking an elderly South Asian woman if she wants help getting out of bed a few times before giving up. The elderly woman may say no because she’s being polite or she’s waiting for a South Asian worker she can speak with in her own language.
Reverence for the elderly is common in many Asian cultures, which can influence how older adults are spoken to. This is one of the things that makes Kooksun Kang, who emigrated from South Korea in 1974, grateful her father was at Rose of Sharon, a Korean long-term care home in Toronto, before his death in April. There are certain ways of expressing things in Korean you can’t express the same way in English, she says. At Rose of Sharon, “the people who work there care about elders — they’re so gentle and patient.”
Kang’s father, Jong Kil Kim, was given a bed three years ago at the age of 100 after waiting a decade. Kim came to Canada after he retired in his 60s, but he loved his independence and lived on his own for many years in an assisted living facility. He had many Canadian friends and enjoyed exercise, going to church and playing golf. Around age 95, Kang started to notice changes in his memory. He’d forget how to turn the TV on or wouldn’t eat food she left for him in his fridge. She was worried about his safety.

Kang is often told that getting a spot at Rose of Sharon is like winning the lottery, and she can see why. She used to volunteer at a mainstream facility near her home in Toronto, and that’s where her father was first assigned. Within two weeks, he refused to stay, confused about why he was being put in a home at all. The following month, Kang got the call from Rose of Sharon. While the transition for her father was still tough, she thinks familiar faces, food and language helped him settle in.
This familiarity also provided her with solace during the pandemic. Kang found it distressing not knowing when she could see him face to face again as the home only allowed weekly visits through a window. She was heartbroken that her father couldn’t understand what was going on. Adding to this stress was Rose of Sharon’s proposed sale to a non-Korean for-profit company last year. She worried about the quality of care her father might receive as a result. After over a year of community protest, a Korean non-profit is poised to buy the home, which is a relief for Kang.
Seong-gee Um notes the wait times for homes like Rose of Sharon are so long that many on the lists die before their names come up. While there are plans to build new homes, demand for ethno-specific care homes will not be met anytime soon. Instead, she says that “culturally competent care should be embedded across the whole long-term care system.” Um hopes this will be part of the process of creating new federal long-term care standards, an initiative announced in the spring and led by Dr. Samir Sinha, director of geriatrics at Toronto’s Mount Sinai and University Health Network hospitals.
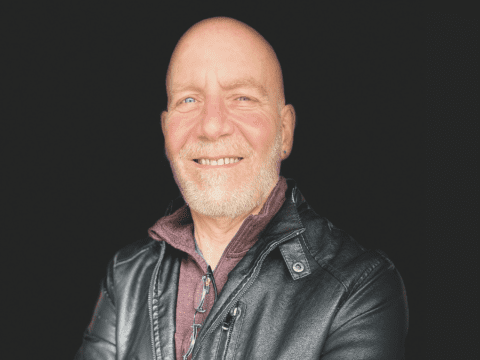
“These homes are not culturally sensitive — the language is different, the treatment is different.”
Jyan Nath
As for Jyan Nath, she’s given up on trying to find a culturally appropriate care home for herself. No such long-term care homes for South Asians appear to exist in Canada, although Ontario approved licences for two in Brampton this year. A few years ago, she spent time looking at 10 homes with her son. Even the most upscale ones didn’t provide what she needed: variety in food and opportunities to practise her religion as a devout Hindu. While she’s open to other spiritual practices, she would like space for her morning rituals and the ability to determine relevant programming, like having a priest who regularly visits for religious discourse. “That should be organized [by the facility], because when you get older and you are in a home you can’t organize for yourself — that is why you are in a home,” says Nath.
Her sister moved in with her right before the pandemic, and for now they’re managing well. Once there’s a lower risk of becoming infected by COVID-19, Nath will rehire the woman who used to help her around the house. She has decided to use some of the money she would have spent on a facility to upgrade her condo: a two-bedroom, 110-square-metre unit with a sweeping view of the mountains from Mount Baker to Grouse. “We see the sunset, and it’s really beautiful here,” says Nath. “This is our last home until we can’t manage anymore.”
***
Sadiya Ansari is a Canadian journalist who often covers issues related to race, immigration and multiculturalism. She lives in Berlin.
CORRECTION: A previous version of this story stated that Momiji is a long-term care home. It is a supportive living facility. This version has been corrected.
This story first appeared in the July/August 2021 issue of Broadview with the title “A Place Like Home.”