Kelly Dunfield wants to make epinephrine auto-injectors (EAI) accessible across North America. Inspired by a heartbreaking story of an allergic reaction turned fatal, the long-time nurse practitioner launched a family-led pilot project in 2014 distributing EAI cabinets to public sites in Sussex, N.B. After initial success, she created Be Ready Health Care the following year, expanding her commitment to community health far beyond the Maritimes. Almost a decade later, Dunfield’s project has saved many lives.
Beginnings
I was at a conference listening to an allergist speak about a young lady who had unfortunately died of a severe allergy. And I was sitting there thinking, “We would have never dreamt that people would be able to use automated external defibrillators in places like airports and shopping centres. Why aren’t we doing this with epinephrine for severe allergies?” Every resource I read said it should be available as a first-line treatment, but nowhere could I find that it was actually being done.
Necessity
Some people know they have allergies but don’t always carry their injectors with them. And although we recommend people carry two injectors if they know they have an allergy, most only carry one. As a result, if someone’s having a severe anaphylactic emergency and needs an epi, they may often need a second dose in five to 15 minutes. The third example is the scariest: a person doesn’t know they have an allergy, and they suddenly develop one. So of course, they would never even dream of carrying an epi with them.
More on Broadview:
- How long COVID is shining a new light on chronic fatigue syndrome
- I was forced into the psych ward as a teen. Now I’m teaching police officers how to respond to mental health calls
- How over-policing Black children can damage their mental health — and future
Barriers
Most people just don’t know how important it is to have this, and I wish that our governments would have a say somehow. The way we’re housing epinephrine kits — whether they’re in your purse or in your pocket, where they’re out of reach — is not good. Making sure they are where they should be is the thing that I would encourage everybody to have a look at and think about. If we have the kits centrally located, visible and accessible at all times, everybody learns where they are, like fire extinguishers.
Want to read more from Broadview? Consider subscribing to one of our newsletters.
Impact
I get calls practically every day. We have the cabinets all across Canada at colleges, universities and restaurants. We have them with people who run their own daycares out of their homes. I always say, “Wherever there are insects, medications and food, there should be an epinephrine kit.” I want to get people to think about it more positively. Wouldn’t you rather have a cabinet than not? It would be the biggest reward of all, really — my heart would just swell if I could see cabinets everywhere I go.
***
Mark Ramzy was an intern with Broadview this summer. Currently a reporter for the Toronto Star, he lives in Ottawa.
This article first appeared in Broadview’s December 2023 issue with the title “Kelly Dunfield: Nurse.”
Thanks for reading!
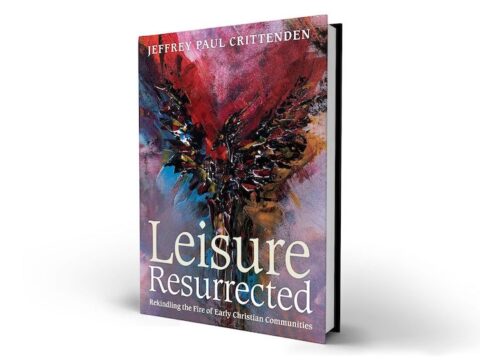
Did you know Broadview is the only media organization in Canada dedicated to covering progressive Christian news and views?
We are also a registered charity and rely on subscriptions and tax-deductible donations to keep our trustworthy, independent and award-winning journalism alive.
Please help us continue to share stories that open minds, inspire meaningful action and foster a world of compassion. Don’t wait. We can’t do it without you.
Here are some ways you can support us:
Thank you so very much for your generous support! Together, we can make a difference.
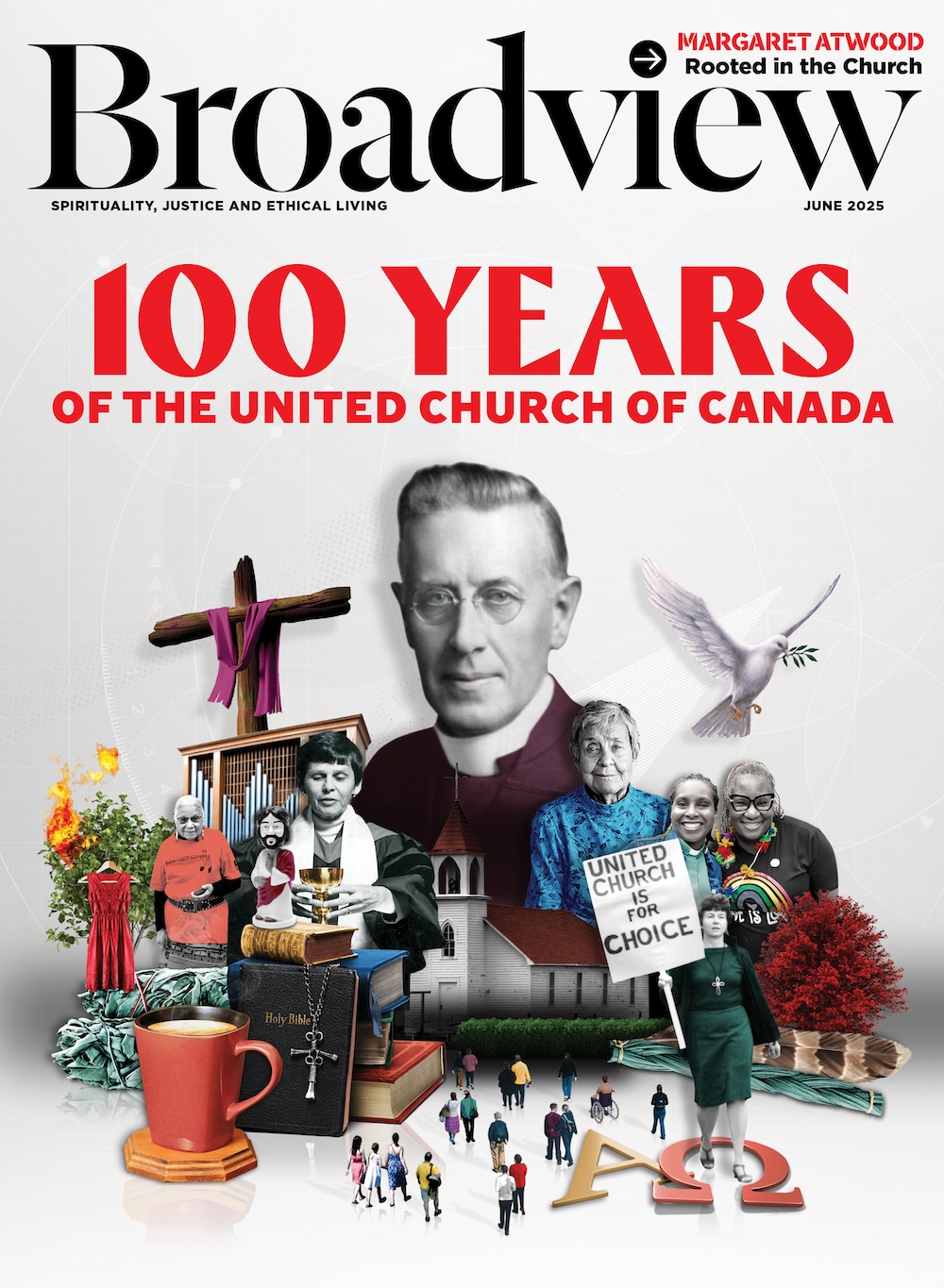
Jocelyn Bell, Editor/Publisher, CEO and Trisha Elliott, Executive Director