In 1513, when the Spanish explorer Ponce de León was searching for the fabled fountain of youth, he went to Florida. After wading through malarial swamps, the legend goes, he came upon some disease-free spring water around what would become St. Augustine. He declared it the fountain of youth, and it became his fame. Five centuries later, when I am looking for something similar — an explanation for aging and an answer to the question of whether we might do something about it — I get on a plane for California. My destination is the Buck Institute, a stunning building of glass and white travertine stone designed by I.M. Pei and set like a jewel on 200 hectares of wooded hillside in Marin County, north of San Francisco.
In 1900, the average life expectancy for a Canadian was 50. Some, of course, lived much longer, but those who died as infants or in childbirth or of various infections kept down the averages. By 1990, with improved sanitation, antibiotics, vaccines and better practices during childbirth, average life expectancy had risen to 74 for males and 81 for females. By 2012, it was 77 and 82. Could it improve any further? The low-hanging fruit has already been plucked. Further gains would require crossing a new frontier: making old people live even longer — perhaps dramatically longer.
You may unsubscribe from any of our newsletters at any time.
The Buck Institute bills itself as the world’s leading private institution dedicated to the study of aging, and its scientists even coined a term for their investigation — “geroscience.” They dare to ask: Why do we age? And is it possible to slow, stop or even reverse that process? The questions challenge assumptions that hold sacred places in our culture: that aging is a natural and inevitable process, and death is as certain as taxes. How much should we tinker with what most of us believe is a set limit to the human lifespan?
As I started my research, I felt unsettled. Apparently I’m not totally enthralled about the possibilities of science transcending nature. I couldn’t escape a feeling of disloyalty to the proper rhythms of the universe. The Psalmist pegged the ideal human lifespan at threescore years and 10, or even fourscore for the strong (that’s 70 or 80). We are told that Moses lived to 120, Noah to 950 and Methuselah to 969. But I always assumed those numbers were exaggerated — or somehow from a different calendar. The longevity record in modern times is 122, held by a French woman named Jeanne Calment, who died in 1997.
It’s hard to argue that longer life is a negative thing. Yet there have always been opposing camps. Aristotle described the elderly as those whose “passions have slackened, and they are slaves to the love of gain.” The centuries-long quest to turn nature on its head has included some wacky practices, such as implants of goat testicles and ingestion of radium-laced elixirs. In 1934, poet W.B. Yeats emerged from what was in effect a vasectomy at age 68 claiming to be frisky as a colt. Scientific research into aging has roots in the 1960s, but it got going in earnest in the early 1990s with a generation of scientists who remain active today — several of them at the Buck.
***
The Buck Institute was established by the estate of Marin County philanthropists Beryl and Leonard Buck. Leonard, a pathologist whose family owned an oil company, died in the 1950s. His widow, Beryl, died in 1975 expressing the desire “to extend help towards the problems of the aged.” Twenty-four years and several lawsuits later, the Buck Institute opened its doors, funded by income from the estate. Kris Rebillot, director of communications, explains that 17.5 percent of the institute’s present annual budget of US$32.5 million comes from the Buck Trust. To support the work of the 229 employees, each of the 23 faculty augment this funding through grants.
Rebillot takes me below the gleaming upper floors into an underworld of laboratories chock full of expensive equipment. Microscopes, freezers and cell-sequencing apparatus share space with thousands of research subjects: mice and fruit flies, yeasts and microscopic worms. These tiny specimens are where the strategies that will someday be applied to humans are tested. Institute CEO Brian Kennedy has spent the past 25 years looking through his microscope at yeast. His colleague, Gordon Lithgow, has spent equivalent time with tiny worms called C. elegans. Judith Campisi and her post-doctoral students work with mice, while Pejmun Haghighi spends his days with fruit flies. It’s not that we are reduced to these tiny beings, but the other way round: to understand how the cells in more complex beings function, you need to start with the single-cell organisms and work up.
Geroscience is different from research into the various diseases that hit us when we get old, though Haghighi (who is also on the faculty of McGill University in Montreal) looks for clues to Alzheimer’s in the proteins of his fruit flies, and Campisi (who has a posting at the University of Alberta by virtue of supervising one of its PhD students) hopes to postpone age-related cancer through what she is learning from the cells of her mice. Geroscience also differs from gerontology, the examination of everything to do with aging, including the socio-economics.
Lithgow, a Scot who maintains his soft brogue, explains that the beauty of his worms is their 20-day life cycle. “Things go on in the worm during those 20 days that take 80 years in us.” The highlight of his career came in 2000 when he and a colleague changed a single gene and managed to make one of their worms live not for 20 days, but 40.
Campisi cranks up a PowerPoint presentation to explain what she has learned about how our cells age and the mischief that leads to heart and vascular conditions, neuro-degeneration, diabetes, organ failures, osteoporosis and cancer. “The occurrence of these diseases rises exponentially after age 50 or 60, and the evidence is mounting that there is something about the process of aging itself that is driving them all,” Campisi says. “That is our hypothesis, and if we’re right, we will absolutely revolutionize modern medicine.”
What she predicts is that the silo model, where specialists look at one disease at a time, will collapse and geriatricians will instead treat aging itself. The focus will be on avoiding or postponing disease by creating a generally more healthy body that deteriorates more slowly. “It’s still a dream that we will be able to tackle diseases in this way,” Campisi adds, “but it’s no longer science fiction.”
What Campisi, who hails from New York, has figured out over 35 years is that as we get older, multitudes of useless “senescent” cells impede our bodies from attacking all the above-mentioned diseases. In collaboration with colleagues at the Mayo Clinic, she has been able to inject powerful drugs that help mice get rid of senescent cells and, as a result, clear their bodies of cancer tumours. It’s only a matter of time, she believes, until drugs achieve the same for humans.
***
Integral to many theories of longevity is something called caloric restriction (CR). In the 1930s, scientists at Cornell University observed that severely restricting dietary calories in lab rats — while maintaining micronutrient levels — resulted in life extension. In subsequent decades, experiments have been carried out with dogs and primates, in all cases achieving extended lifespans.
Severe calorie restriction, however, has side effects. No one wants to feel cold and experience slower healing of wounds or reduced sex drive, acknowledges Brian Kennedy. “People don’t want to be malnourished, and few want to put in the effort to gather the knowledge to do it [CR] properly. You can’t eat two Snickers bars and call it a day.”
The trick, then, is finding a drug that will mimic what was achieved in the rat studies while letting humans continue to eat normally — what’s known as a “mimetic.” Writer David Stipp, whose book The Youth Pill details research initiatives into human aging, states that CR mimetics from the early 2000s began “to transform the anti-aging quest from an endless guessing game into a fairly routine exercise in drug development.”
Some initiatives have stumbled after promising debuts. An exciting moment in the early 1990s was identifying the so-called French paradox: despite rich diets loaded with sauces and cheese, the French were discovered to have healthier hearts than Americans. Could it be because of the red wine they consumed?
Researchers soon isolated an ingredient called resveratrol. When tested on yeasts and finally on mice, it extended both lifespan and energy. Then it was acknowledged that the average person would have to drink 300 glasses of wine per day to replicate the dosage and effect.
Something currently considered promising is rapamycin, a member of a class of drugs called mTOR inhibitors, and already shown to be capable of counteracting aging and delaying age-related diseases in mice and other animals. This is where Kennedy is directing much of his research energy. In one trial, mouse lifespan increased by 38 percent. In 2014, the pharmaceutical company Novartis proved rapamycin safe for humans through a six-week trial with older people who were also receiving the influenza vaccine. The drug zeroed in on a genetic signalling pathway associated with immune function and aging, and improved the participants’ immune reaction to a flu vaccine by as much as 20 percent.
The 25 years of Kennedy’s scientific career match the trajectory of modern aging research. Now 51, the Kentucky-born scientist has been, since 2010, CEO of the Buck Institute after stints at MIT in Boston and the University of Washington in Seattle. “Skeptics have always argued that aging is a natural process, and you could never test drugs for aging in humans because you shouldn’t give drugs to healthy humans,” he says. He sees the work of his colleagues, both at the institute and in the increasing number of research programs in universities around the world, as preventative medicine.
“We don’t want people living longer if it’s just prolonging their time suffering the diseases of aging. We want to see if we can delay or postpone those. People imagine we’re trying to make rich people live longer. We’re not doing anything different than people targeting one disease at a time. We’re just trying to come up with an intervention that will prevent multiple diseases at one time, something that will prevent cancer that, by the way, might also prevent Alzheimer’s.”
***
While the Buck Institute scientists seek pharmaceutical keys to extending longevity, that goal has already been achieved elsewhere through more natural means. A decade ago, National Geographic writer Dan Buettner set out to find “blue zones,” places around the globe where people seemed to live extraordinarily long lives — naturally. Buettner identified five: a corner of the Mediterranean island of Sardinia, Okinawa in Japan, Ikaria island in Greece, the Nicoya Peninsula of Costa Rica and — the next stop on my journey — Loma Linda, Calif.
Each blue zone community had its defining characteristic. What distinguishes Loma Linda is the fact that most of the 23,000 people who live there are Seventh-day Adventists — the church founded in the 1860s that, among other things, follows Old Testament rules (no tobacco, alcohol or pork) and observes a strict Saturday Sabbath. Adventists are also deeply committed to health, having established hospitals all over the world. One of their largest health-care facilities is in Loma Linda where, in 1905, Ellen G. White founded a nursing school that became Loma Linda University; a community grew up around it. White’s 1905 book, The Ministry of Healing, became a bible of proper nutrition.
Well before the arrival of Buettner, Adventists realized they had something special going on. In 1960, 23,000 Californian members of the church joined the Adventist Mortality Study. Through it, they discovered that if the death rate from coronary heart disease in non-Adventists is taken as 100 percent, then deaths among Adventist men were only 66 percent of what was expected (and 98 percent for women). Overall cancer deaths, again with the non-Adventist population as the standard, were 60 percent for Adventist men and 76 percent for Adventist women. Mortality was also lower with specific types of cancer: the lung cancer death rate among Adventists was 21 percent; the colo-rectal cancer death rate was 62 percent; the breast cancer death rate for Adventist women was 85 percent; and the prostate cancer death rate for Adventist men was 92 percent.
In 1974, another study of 34,000 California Adventists began, this time to determine what components of their lifestyle contributed to the lower rates of diseases. Yet another study was launched in 2002, with 96,000 Adventists from across the United States and Canada. This one, which is still ongoing, is exploring the links between lifestyle, diet and disease.
Larry Beeson is a cheerfully relaxed professor at Loma Linda University’s School of Public Health. The 68-year-old, who sports steel-framed glasses and mutton-chop whiskers, classifies himself as a “lifer.” Beeson came to the university as a student and was welcomed onto the faculty in 1973. He’s been there ever since, teaching generations of students and joining the research into their one big question: Why do Adventists live to such a ripe old age? Male Adventists outlive other men in California by 7.3 years, and female Adventists outlive other women by 4.4 years. And not, emphasizes Beeson, seven and four dragged-out years but, by and large, vigorous, healthful, productive years. “We die in the end of the same diseases — heart and stroke and cancer — but we do it later and live well up until that end.”
Adventist studies compare the health and longevity effects of various diets. Beeson (who consumes eggs and milk but not meat) notes that vegans have the lowest rates of Alzheimer’s disease and dementia, a number that climbs as more animal products are introduced. A vegetarian diet is recommended for church members but not enforced. The culture of the town supports such a lifestyle with lots of vegetarian options and soy milk on restaurant menus and in grocery aisles. School cafeterias are vegetarian.
The conclusions of the studies reveal no mysteries to someone like Beeson who rhymes off the essentials: “Eat a plant-based diet; maintain normal body weight — avoid being obese; don’t smoke or drink, except lots of water; eat lots of nuts; maintain a faith base — bring God into the picture.”
This last point particularly intrigues him. “When Dan Buettner came here,” Beeson observes, “the one thing that separated Loma Linda from the other blue zones was the 24-hour Sabbath. That is, the time to de-stress, put my work aside and replace it with concentrating on my relationship to God, to my family, to my friends.” In the current ongoing health study, a sub-study, designed by psychologists and members of the faculty of religion, will try to quantify the effect of being a religious practitioner on health and longevity.
What is it like to live in a town with a substantial population of seniors? As I drive around the spanking-clean streets, I note that the civic centre is promoting a scrapbooking workshop for seniors. The organic produce supermarket has basket-mounted scooters for mobility-challenged customers, as does the campus food market. But this is not a seniors’ community like you might find in Florida; Loma Linda is definitely mixed. When I peek in the door of the university gym (which is open to the public), I note as many grey-haired persons as students sweating on the machines. While seniors make up 14 percent of Loma Linda’s population (compared to the California average of 11 percent), there are also the 4,500 students at its medical schools (many of whom are Asian), as well as the university’s faculty and staff members and their families. It is not a homogenous place.
Except in the religious sense. Rev. Randy Speyer, one of 17 pastors at the 6,500-member Loma Linda University Church, tells me that there are almost no churches other than Adventist inside the town limits, and 30 more Adventist churches in a 10-mile radius beyond the town. With those kind of numbers, it’s not hard to keep the Sabbath customs. Speyer spent 20 years as a counsellor in northern California before coming to Loma Linda’s church last year.
This is the first time he’s been in such a monolithic community, as well as one with such a preponderance of older people. Five of LLUC’s 17 pastors are dedicated to ministries with seniors. But some noteworthy things are observable: the generations mix, and seniors teach children in Sabbath school. Seniors also take leadership roles on committees and are committed to continued education. When people are spry and vigorous in their 80s and 90s, it redefines the term “seniors.” Lots of 65-year-olds, Speyer observes, remain working as teachers and doctors, enjoying their professions and the contributions they make.
As a man of a certain age, I’ve decided to embrace John Burroughs’s dictum that “old age is always 10 years older than I am.” Yet, although I’d be happy to see aging postponed, I also feel I must be prepared to gracefully leave the stage — not hog it at the expense of those coming after me. Nothing in the healthy mix of generations in Loma Linda, nor in the modest and reasonable goals of the Buck Institute scientists, offended that instinct. As Kennedy assured me, they’re not trying to make “rich people live longer.” In fact, they know they have big challenges still ahead.
Lithgow acknowledged that what has most surprised him in the 15 years since the eureka moment when his worm doubled its life is how slowly things have moved. “I guess we thought that would be a watershed moment and the walls would come tumbling down,” he said. “Money would come into the field; pharmaceutical companies would pop up recognizing that aging and disease were going hand in hand. It didn’t happen.” Instead, geroscience remains at the edge of respectability, with the pharmaceutical industry slow to invest because government regulators aren’t yet on board with anti-aging drugs.
“The complexities of humans still encompass huge unknowns,” Lithgow admitted. “There are holes in our understanding. The big challenge remains translating what we know from studying worms into something of import for humans. That is painstaking, time-consuming and expensive.”
Coincidentally, while I was travelling through California last February, Time magazine put human aging in the public eye, featuring a baby on its cover with the provocative headline, “This baby could live to be 142 years old.” The sensational pronouncement played into the hands of enthusiasts, who love to trumpet the possibilities of 90-year-olds who look and feel 45.
We already do take some things for granted. Today’s medicine prolongs life each time it treats or cures an individual’s disease. But will a combination of drugs and geroscience prolong life for the population as a whole? What about the more extreme possibilities of turning back the clock — actually making people younger?
This has already been achieved in the labs: blood from young mice has been transfused into old mice, heralding a futuristic horror show where the old, like vampires, might feed on the young. And despite Lithgow’s gloominess about financing, some very big players are showing up. In 2013, the Internet giant Google set up Calico (California Life Company) with an investment reputedly in the range of $1 billion. The specifics of Calico remain secret, but its project is generally to “harness advanced technologies to increase our understanding of the biology that controls lifespan.”
This brought me rudely back to reality. Science will plow forward, but so will the accompanying implications. In her lead essay in Time, Laura Carstensen, founding director of Stanford University’s Center on Longevity, postulates that “our aging society presents challenges every bit as fundamental and pervasive as climate change and globalization.” Carstensen’s centre, established in 2006, has charted how quickly the demographic structure has been reshaped. Once a pyramid, with a small quotient of elderly at the top, it now looks more like a rectangle, with the aged population equal in number to the young.
The implications of this shifting demographic are both financial and structural (things like architecture with no stairs or automobiles that drive themselves). But they’re also ethical. How will the changing demographics affect things like global population pressures, demand for resources and political tensions between the young and the old?
The idea of a fountain of youth retains its imaginative power, and the possibilities are more enticing than ever. But the issues at play are not simply scientific. And we’re going to have to start talking about them.
***
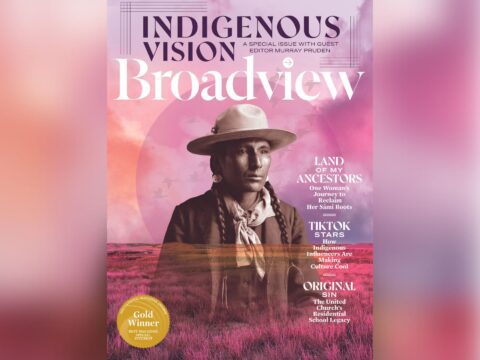
This story first appeared in The United Church Observer’s May 2015 issue with the title “Forever young.”