Jan Brenner is a 30-ish gallery curator who lives with her husband in the well-to-do Alberta enclave of Bragg Creek. She counts oil barons and sports heroes among neighbours drawn to the area by the clean alpine air, million-dollar sunsets and easy commutes to Calgary and the mountain playground of Kananaskis.
Jan mostly observes life in Bragg Creek from a distance. She suffers from a condition that saps her energy, muddles her thinking and causes pain that often confines her to a lounger on her deck where, wrapped in an afghan, she watches the world through a pair of binoculars. She takes stimulants when she wants to feel like her old self, but she knows the crash afterwards will be brutal.
You may unsubscribe from any of our newsletters at any time.
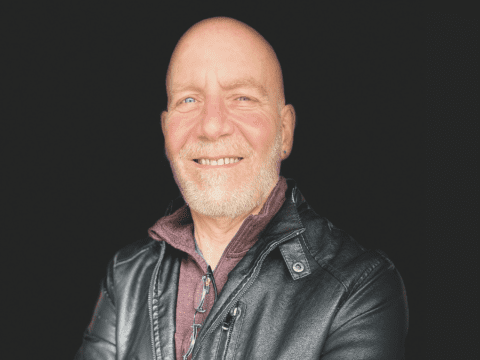
Bragg Creek is real. Jan Brenner isn’t. She’s a character created by Calgary crime novelist J.E. Barnard for a trio of mysteries set in the Alberta foothills. Barnard’s first name is Jayne, and it’s no accident that she gave Jan a name that sounds like her own. She, too, is ill much of the time, with symptoms that mimic the worst of Jan’s and then some. It has taken a titanic effort on her part, and the support of those close to her, to fashion a career as a writer.
“I was in pain continuously for months at a time,” she recalls as she describes the challenges of writing. “Just to meet the deadline, I read nothing, spoke of nothing and watched pretty much nothing. I couldn’t keep all the pieces of the novel in my head if I had to also answer questions about a grocery list.”
Barnard decided to insert Jan Brenner into the first novel of the series, When the Flood Falls, after a five-year low ebb that she barely survived. “I said, I have to write her into this novel as a real person who is struggling with this illness because it may be the only book I’ll ever write.”
About halfway through When the Flood Falls, Barnard names the illness she and her character share: myalgic encephalomyelitis (ME), also known as — and some say trivialized by — chronic fatigue syndrome. Barnard is among an estimated 580,000 Canadians living with ME. The disease, which has no known cause or cure, is recognized as a complex chronic illness by health authorities, yet only a handful of doctors can claim to be ME specialists, and most medical schools don’t include it in their physician training programs.
Like a lot of people with ME, Barnard has been living with the illness for a long time — in her case, more than 30 years — as well as the stubborn perception that ME is a phantom disease more in the minds of patients than in their bodies. She spent years pretending she had a blood sugar deficiency to avoid the stigmatization that spawned epithets like “yuppie flu” and “shirker syndrome.” She still encounters it. Barnard says her publisher insisted that she dial back some of the harsher details of Jan’s illness, telling her, “This is too depressing. She sounds whiny.”
Despite ongoing research and some limited progress in the treatment of symptoms, people afflicted with ME are still often perceived as weak-willed or mentally unstable. Things might change if the disease were to find a way into the medical mainstream. For years, the ME community has wondered what it would take for that to happen. Recent events may have provided the best answer yet: a pandemic.
ME has been dubbed the “disease of a thousand names,” some of them reflecting the scorn that has haunted sufferers for centuries. In the 1700s, the symptoms now associated with ME were described as a “nervous or hysteric fever.” A 19th-century American neurologist conjoined the Greek words for “nerve” and “weak” to come up with the label “neurasthenia,” attributing the condition to advances such as “steam power, the periodical press, the telegraph, the sciences and the mental activity of women.”
Since then, the disease has been named and renamed with a regularity that underscores the unsolved mystery of its origin and a fierce debate over its physical or psychological nature. Sometimes it would be linked to the location of an outbreak — for example, “Iceland disease” or “Otago mystery disease” — or to existing ailments such as rheumatism, polio and Epstein-Barr syndrome. One magazine called it “Raggedy Ann syndrome” after an outbreak in Lake Tahoe, Nev., in the mid-1980s. Later that decade, the U.S. Centers for Disease Control and Prevention adopted the term “chronic fatigue syndrome” (CFS) to describe “a syndrome of unknown cause characterized primarily by chronic fatigue.”
Ongoing research is probing links between muscular pain, or the myalgic aspects of the illness, and inflammatory conditions in the brain and spinal cord — encephalomyelitis. Since 2017, the U.S. Centers for Disease Control and Prevention has used ME and CFS interchangeably. Health Canada and other public health agencies have followed suit. Even so, the designation hints at subtle stigmatization. As an international panel noted in 2011, “No other fatiguing disease has ‘chronic fatigue’ attached to its name — e.g. cancer/chronic fatigue, multiple sclerosis/chronic fatigue — except ME/CFS.” The panel declared, “It is more appropriate and correct to use the term ‘myalgic encephalomyelitis’ (ME) because it indicates an underlying pathophysiology.”
ME tends to be most common in adults aged 40 to 60, and women are more affected than men. But it can strike anyone at any age, at any station in life. Florence Nightingale and Charles Darwin may have suffered from it. Pop stars Cher and Stevie Nicks and jazz virtuoso Keith Jarrett have it. Symptoms can fluctuate. In severe cases, patients are unable to tolerate light, sound or touch. The hardest hit are completely bedridden and tube-fed.
Although in some cases the onset of ME follows a viral or bacterial infection, the mechanism that triggers it is unknown, nor is there a specific test for diagnosing it. Instead, a diagnosis of ME involves a lengthy process of ruling out other conditions while identifying certain core criteria: a lingering inability to engage in pre-illness levels of activity; post-exertional malaise, or the worsening of symptoms after even minor amounts of physical or mental activity; unrefreshing sleep; cognitive impairment; and dizziness that intensifies when standing up after sitting or lying down. Related symptoms range from heart problems to digestive difficulties.
It’s one thing to enshrine diagnostic criteria; it’s another to get diagnosed. One day last winter, Ryan Kirkness ventured out of his home in Winnipeg to attend his daughter’s ringette game. He knew he would pay a price for his effort. The next day, he was sore. Kirkness, 50, survived a bout of aggressive testicular cancer 20 years ago. Chemotherapy left him with nerve damage and debilitating pain.
About four years ago, Kirkness began to experience post-exertional malaise. He suggested to his family doctor that he might have ME and that it might be linked to the rigours of chemotherapy. The doctor told him he knew nothing about ME and was less than receptive when Kirkness showed him a brochure prepared for physicians by the Manitoba ME support group. “It was kind of like, ‘Oh, you think you can diagnose yourself?’” Later, during the throes of the COVID pandemic, Kirkness approached his doctor again, who told him, in so many words, that he wasn’t able to help him. Like thousands of patients elsewhere, Kirkness ended up drawing on the experience of others, particularly those in the Manitoba ME support group, to conclude on his own that he has the disease.
Maria Moores helps to administer the Manitoba group. At 28, she’s been sick for more years than she’s been healthy. Moores, who lives in the south-central Manitoba town of Manitou, says she figured it out herself in 2010 that she had ME, but it wasn’t until 2015 that she “finally found a doctor who was willing to name it.” She says her experience in the medical system left her traumatized. “Time and again, you’re told it’s in your head, and you almost start to believe it.” Kirkness, too, confesses that the doubts of others can make him doubt himself; in his darkest moments he considered medically assisted dying.
Surveys by Canadian ME support groups have found that patients report, in the words of a recent study in British Columbia, “a high level of stigma and/or dismissal at many interfaces within the healthcare system.” This echoes the findings of a 2022 paper published in the Journal of Health Psychology. Citing an earlier study comparing ME patients with those suffering other chronic illnesses, the paper notes that “the 42 participants with ME/CFS reported higher levels of perceived stigma than all other participant groups.”
Moores and Kirkness are among an estimated 18,000 people in Manitoba living with ME. Like Kirkness, most are undiagnosed. Many who have been diagnosed have had to travel hundreds of kilometres to see a qualified doctor — if they can get an appointment. Until her recent retirement from clinical practice, Dr. Eleanor Stein of Calgary was one of only two ME specialists in the Prairie provinces.
By the time she saw them, many of her patients were at their wits’ end. “It’s not uncommon for me to have seen a patient who had been to 10 specialists,” she says, “and none of them were helpful….All they did was rule out of their little individual ivory towers: ‘You don’t have kidney disease; you don’t have heart disease; you don’t have autoimmune disease, endocrine disease.’ Because the doctors don’t know anything about ME, they weren’t able to actually say what they did have.”
Stein could empathize with her patients. In 1989, two years out of medical school, she fell ill and was diagnosed with chronic fatigue syndrome. While she had the skills and network to navigate the medical system, she knew most people did not. Seeing the urgency of the need, she decided to devote her career to helping others with the illness. “Literally, the day I opened my practice I was full,” she says.
Stein guesses that there are no more than 10 ME specialists in all of Canada, reflecting data showing that Canadians with ME report the highest levels of unmet health-care needs in the country. Most ME specialists work out of clinics in Vancouver, Toronto and the Halifax region. “So unless you live close to one of those clinics, you basically have no care at all,” she says.
More on Broadview:
- Peer support workers could be a solution to Canada’s surging mental health needs
- Malawi’s ‘faith healers’ are leading HIV-positive people to reject treatment
- How these Amazing Race Canada winners overcame adversity through faith
The remedy seems obvious: train more specialists. Dealing with ME-type illnesses was not part of Stein’s own medical training. Forty-plus years later, she finds it “appalling” that most newly minted doctors in Canada start their clinical careers with virtually no exposure to ME. “It was on the curriculum at the University of Calgary only because I harassed them every single year. I got one hour. Now that I’m retired, I strongly suspect it will not be covered anymore.”
The U.S. Centers for Disease Control and Prevention acknowledges that “most medical schools in the United States do not have ME/CFS as part of their physician training” and that “the illness…might not be taken seriously by some health-care providers.” A paper co-authored earlier this year by Dr. Hannah E. Davis, a prominent American microbiologist and patient-led research advocate, noted that some poorly trained doctors “still advise patients to pursue harmful interventions,” including psychologically focused therapy and graded exercise, “despite the injury that these interventions cause and the fact that they are explicitly not advised as treatments.”
***
Christmas 2021 was a bust for the Krotz Adams household in Edmonton. Both parents and their two adolescent sons came down with fever, coughs, aches and exhaustion. Tests for COVID-19 were scarce, but the surge in the Omicron variant in the weeks leading up to the holiday convinced Sarah Krotz and her husband, both professors at the University of Alberta, that they had contracted the disease that by then had infected nearly 280 million people worldwide and claimed 5.4 million lives.
The symptoms eventually ran their course, but then 11-year-old Fen Krotz Adams developed a wicked cough, chest pains, chills, headache and persistent, crushing fatigue. Visits to the ER and the family doctor, as well as X-rays and blood tests, showed nothing out of the ordinary. Fen was referred to a pediatrician who advised sending him back to school part time. That only worsened his symptoms, so the pediatrician recommended, to his mother’s dismay, the antidepressant drug Prozac. A second pediatrician couldn’t pinpoint a diagnosis either but referred Fen to a psychologist who works with kids struggling with long-term diseases.
Throughout, Fen’s parents charted his ups and downs and put their research skills to work trying to answer what the doctors couldn’t. “Once we ruled out a whole bunch of other possibilities,” says Krotz, “we finally came around to the fact that this was tracking like textbook long COVID.” The psychologist came to the same conclusion, recommending a program of paced activity and rest often prescribed to people with ME. By September 2022, Fen was able to go to school three days a week. By October, he was back full time but more prone than usual to seasonal viruses.
When he took sick, Fen was among an estimated 32 million people worldwide classified as COVID long-haulers; the number as of January was 65 million and counting. Like ME, long COVID appears to be triggered by an infection — COVID itself — and many of the common symptoms, including exhaustion, brain fog and post-exertional malaise, are also core symptoms of ME. Long COVID, like ME, affects women more than men. Prominent researchers such as Dr. Mady Hornig of Columbia University think long COVID might be ME by another name.
Early on, long COVID provoked the kind of gaslighting that has plagued ME sufferers for decades. Some of the first studies theorized that long COVID often indicated underlying mental health issues more than it did physiological ones. A 2021 article in the Wall Street Journal went so far as to suggest that long COVID “is largely an invention of vocal patient activist groups.”
Long COVID has since merged into the mainstream. Spurred by studies projecting an economic impact in the trillions of dollars and by fears that the surge in cases could overwhelm health-care systems, research efforts have kicked into high gear. The National Institutes of Health in the United States is spending US$1.5 billion on long COVID projects through 2025. This spring, Canada’s chief science adviser warned of a “mass disabling event,” and the federal government announced $29 million in funding to develop clinical guidelines and create a national online network for researchers and clinicians.
About half the people diagnosed with long COVID meet the diagnostic criteria for ME, raising the possibility that ME could ride long COVID’s coattails to more legitimacy in the medical establishment. It’s also possible that long COVID research could spin off clinical benefits for ME patients.
Dr. Kieran Quinn of Toronto estimates that there are as many as 1.4 million people with long COVID in Canada. Quinn served as assistant director of the Ontario COVID-19 Science Advisory Table shortly before the province disbanded it in September 2022. He is currently helping to spearhead a clinical trial that aims to discover new treatments to improve the quality of life for people living with long COVID. While not the focus of the trial, ME will be very much on the project’s radar. “The hope is that there’s some shared biological and pathophysiological mechanisms across those two conditions,” he says of current research in the field, “such that if we discovered treatments for long COVID…[we] will be able to help a lot of people with ME.”
One organization studying long COVID and ME is Open Medicine Foundation Canada, which funds the ME/CFS Collaborative Research Center in Montreal. Such research will potentially boost the tools physicians have at their disposal, perhaps fostering a more empathetic bedside manner. Quinn observes, “I can’t imagine what it would be like to show up to your trusted health-care provider and have them tell you, ‘This isn’t real. It’s all in your head.’”
Quinn has had patients come to him with fatigue symptoms and leave with a diagnosis of both long COVID and ME. He notes that “it’s not just that long COVID is going to help the ME/CFS world, but the ME/CFS world has helped us a lot already to understand post-viral syndromes.” For the moment, he says, the key takeaway is, “There’s hope on the horizon.”
***
Even toned down, Jan Brenner is in a bad way when Jayne Barnard introduces her to readers in the third chapter of When the Flood Falls. She’s unkempt, barely able to stand up and disruptive. The novel’s protagonist, an ex-RCMP officer named Lacey McCrae, nicknames her “Shaggy” and writes her off as a drug addict, a malingerer. By the third novel in the series, Jan still struggles with ME but is emotionally stronger because she’s now convinced that her condition is genuinely physical, no matter what the doctors say. Managing her disease, not fighting it, means she spends more time out and about in her wheelchair and less time confined to her lounger. Moving within a circle of trusted friends and supporters, she now helps Lacey solve murders.
Jan’s creator is less sanguine in real life than she is in the pages of her fiction. Like many in the ME community, Barnard has a hard time seeing the hope that Kieran Quinn champions. It can still take years for a patient to be formally diagnosed with ME, and the surge in long COVID threatens to spread scarce clinical expertise even thinner. While ME patients may someday stand to gain from the recent boom in long COVID research, they also know that ME remains a perennial poor cousin when it comes to research specifically geared to their disease.
But perhaps more than anything, it’s the accumulated burden of being told over and over that you’re not sick when you are that weighs heaviest. It didn’t come as a big surprise to Barnard when her publisher asked her to sanitize Jan Brenner. “I was used to having the depths of my suffering dismissed by doctors, by relatives, by former friends,” she says. Desperate to get the novel published, “I scaled her back.”
Barnard is a voracious student of current ME research. She wants to believe that the nexus of long COVID and ME will yield improved outcomes for patients with both diseases. But after the better part of a lifetime shadowed by doubt and disbelief, she finds it hard not to be cynical. “What I’m hearing from the long COVID patient community is that increasingly the treatments being pushed at them are the same, or updated versions of, the psychologizing, victim-blaming ones that have plagued the ME community for decades.”
For medical researchers, long COVID is like a giant real-time laboratory for studying post-viral illnesses. But delving into the overlap between ME and long COVID needs to go beyond test tubes and microscopes. Coming to grips with ME means confronting the scourge of stigmatization — it’s as much a part of the disease as its physical symptoms. And its scars run deep.
***
David Wilson is a journalist in Toronto.
This story first appeared in Broadview’s September 2023 issue with the title “Invisible Illness.”