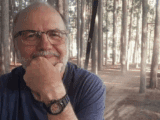
In my family, we joke that my grandpa, Albert Kniesz, is like a cat with nine lives. At 92, he says that by now he’s used up eight of them.
I spent a lot of time with my maternal grandparents growing up. Most of my memories of Albert are set in his shop behind the house he lived in with my grandma in Brunner, Ont., up until he was 90. He had a knack for antique automobiles and spent five years restoring a 1948 Mercury Coupe from a rusty skeleton to a shiny, life-sized toy car. Every morning, over coffee and a bowl of Corn Flakes piled high with brown sugar, he would read the local newspaper cover to cover, carefully archiving each issue in the basement afterwards in case he needed to reference it weeks, months or even years later. Often, he would. He could still recite his first-ever phone number and spoke German on calls with his overseas cousin.
You may unsubscribe from any of our newsletters at any time.
Albert’s life started to look different after an accident in the summer of 2018. While out for a drive on his Ford 8N — his father’s old tractor that he had restored — he was T-boned by a truck at an intersection and thrown several feet through the air. The tractor cracked in half, and somehow he walked away with a mere broken collarbone; cats, after all, are known to land on their feet. Five months later, he ended up back in the hospital with a sepsis infection. The prognosis wasn’t good. They called our family in to say our goodbyes. But the next day, we found him sitting upright in his bed, eating breakfast like nothing had happened. While he did make a full recovery, a chain reaction of health events followed, eventually landing him in an assisted living facility about a year and a half into the pandemic.
A year passed, including our first Christmas not spent together as a family. And then a second. That Christmas morning, my cousins and I trudged through the snow and salt, huddling together in the cold outside my grandpa’s facility in Brunner. My aunt, barely recognizable in her mask and surgical gown, wheeled him up to the window. We couldn’t exchange any words, only a limp wave.
In that moment, it became clear to me how segregated our lives are; there I was, with the entire world accessible to me, while his life was contained inside this tiny waiting room — a real-life purgatory here on Earth. When my grandpa lost his independence, he became a second-class citizen. And despite the fact that growing older and adjusting to life in a changing body is an experience most of us will share, society still largely views aging as a problem. Even a defect.
By 2030, the World Health Organization predicts that one in six people in the world will be 60 or older. By 2050, that will double. The shifting demographics have been referred to as the “grey tsunami,” painting the elderly as an uprising of villains coming to destroy the economy, overrun the healthcare system and jeopardize the futures of younger generations.
Worse, they’re largely written off as burdens. The writers of a 2020 editorial for The Journals of Gerontology noted that those over a certain age are increasingly seen as “helpless, frail, and unable to contribute to society.” The pandemic only amplified that narrative.
My grandfather, however, is far from frail and helpless — he’s the most resilient person I know. But since he went into care, he is different. He no longer reads and often struggles to find his words. Most days, he sits in his room, staring off into space until one of his daughters comes to pick him up for dinner. The joy he once had has been boxed up and stored away in a place that’s hard for him to reach. On rare occasions, he still finds it. His life now is the product of a system that isn’t designed for us to age well. And as we push an entire generation off to the sidelines, that perception of them being unable to contribute in any meaningful way becomes a self-fulfilling prophecy.
But what if we flipped that narrative? What if we stopped thinking of aging as a problem to be solved and instead designed our society in a way that harnesses the wisdom of older generations? The question is one that Stephen Katz, a professor emeritus of sociology at Trent University in Peterborough, Ont., and founder of the Trent Centre for Aging & Society, has spent a lot of time thinking about. “We only have a couple of messages about the future, which are mostly negative,” he says. “But by opening up our reductionist ideas about who and what older people are and can offer…we’ll see that aging in our societies is actually an exciting prospect.”
***
In the Western world, perceptions of aging started to shift around 1880. Before that, when the average life expectancy in the United States was just shy of 40, those who lived long lives were looked up to as beacons of wisdom. But as researchers at the National University of Singapore pointed out in The Journals of Gerontology in 2021, during the Industrial Revolution success became linked with speed and efficiency. The physical shortcomings associated with aging were then seen as a flaw.
Not only did people start wanting to avoid feeling old, but they wanted to avoid looking old, too. As early as the 1900s, beauty companies peddled the idea that their products could slow down the appearance of aging — or better yet, reverse it. Creams and ointments appeared to “fix” every supposed ailment, from balding to wrinkles to grey hair.
The dialogue eventually started to shift in the 1980s, after gerontologists developed the first models of “successful aging,” measured by high physical, psychological and social functioning and no major disease. Television shows like The Golden Girls, which aired from 1985 to 1992, showed that growing older, while it had its challenges, could also be joyful — that is, if you were white, able-bodied and able-minded. Scholars, including crip theorists, have pointed out that these defining qualities shape ideas not only about whose futures are deemed desirable, but also about who gets to participate in society. It’s where ageism and ableism often intersect.
More on Broadview:
- My spina bifida has shaped my life but it doesn’t define me
- How long COVID is shining a new light on chronic fatigue syndrome
- The world and the church have to understand how much they need elder seniors
A survey of more than 83,000 people from 57 countries, conducted as part of the World Health Organization’s 2021 Global Report on Ageism, found that about half of respondents held “moderately or highly ageist attitudes.” This plays out both in the ways we stereotype older people and in how they’re treated. A second survey that took place across 28 countries in Europe in 2014 found that more than one in three respondents aged 65 years or older had been insulted, abused or denied services because of their age.
The pandemic intensified those ageist attitudes and also made them far more visible. “Social indifference to the fact of older people dying became so prevalent, it impeded timely distribution of resources. Some surmised that if children had been dying at unprecedented rates, mitigation would have been swift,” Sandy Grande, a professor of political science and Native American and Indigenous studies at the University of Connecticut, said in a 2022 lecture at Trent University. According to Statistics Canada, those 65 and older account for 93 percent of COVID-19 deaths, totalling more than 21,000 in Canada between March 2020 and May 2021 alone. “The lives of older adults have been at best deprioritized and at worst, deliberately sacrificed,” Grande said.

The effects of ageism on a person’s physical and mental health can be enormous, with victims far more likely to experience loneliness, longer recovery times from illness, reduced quality of life and even premature death. One 2017 German study, which followed 8,000 people over several years, found that those who had negative self-perceptions about aging also had accelerated rates of cognitive decline. Similarly, Chinese researchers estimated in 2017 that older people with negative perceptions of aging had a nearly 20 percent higher likelihood of dying during the six-year observation period.
All of this comes at an economic cost the World Health Organization puts at billions of dollars, since those affected by ageism are also more likely to struggle with financial insecurity, poverty and the subsequent negative health consequences. This not only increases dependency on welfare but also, ironically enough, puts additional pressure on the health-care system.
So if social and physical environments play a big role in determining how people age, what would it take to reshape ours?
***
Japan has the highest proportion of older people in the world. Today, more than a quarter of its population is over the age of 65, and by 2065 that’s expected to rise to nearly 40 percent. In some rural communities across the country, playgrounds are quiet and elementary school classrooms sit empty. One isolated mountain village on the island of Shikoku, known as “scarecrow village,” has no kids at all. After the last students completed Grade 6 in 2012, the school closed down. Now, dozens of life-sized dolls occupy its desks instead.
But rather than fear what’s to come, Japan has rethought its approach to aging altogether. The government is implementing several measures to create what it refers to as an “age-free society,” where seniors are better integrated into both city infrastructure and day-to-day life. The initiatives aim to promote the success not just of the elderly but of all generations.
The coastal city of Toyama repurposed old train and tram lines into a light-rail system with accessibility in mind. Ridership among those in their 60s and 70s more than tripled. In other parts of the country, infrastructure adaptations include barrier-free access to public buildings, repurposing unused classrooms into care facilities and community spaces, and creating more sidewalks with dropped curbs and “tactile paving” to help guide those who are visually impaired. These changes allow seniors not only to continue participating in the workforce if they choose but also to enjoy more active lifestyles.

Most recently, the Japanese government invested in developing a nationwide “community-based integrated care” system. It aims to create a more cohesive network of health care, nursing care, illness prevention, housing and livelihood support to al- low seniors to continue living in environments that are familiar to them. After the first system was launched in the then rural town of Mitsugi in the 1970s, where the elderly population was growing faster than in the rest of Japan, both the proportion of bedridden people and medical costs for the elderly decreased.
Canada, by contrast, designs its suburbs around young and active families who drive vehicles. They have green spaces for people to walk their dogs and endless coffee shops. “There is very little vision that asks what happens when these people grow older,” says Katz. Without adequate public transit, wheelchair and walker-friendly sidewalks, and age-friendly activities like exercise groups, more seniors end up stuck at home or are even forced to leave their communities. Those people, Katz adds, are often the ones who end up in long-term care, where they become even more isolated.
The message in our towns and cities is clear: young people are the future, and older people are the past. But when an entire generation becomes an afterthought, the result isn’t just a lack of visibility — it also negatively shapes our perceptions of what it means to age. Katz says that when he teaches aging classes, he always asks his students how old they can imagine being while still being themselves. Most of them say 65. “There’s no blueprint beyond that; no model of life that looks attractive into the last third of life,” he tells me over Zoom.
His sentiment is echoed by Anna Harvey, a Victoria-based retirement coach who launched her business, Retire Solo, last year on her 70th birthday. “When you think about it, there’s social scripts for every other life transition that we go through,” she says, listing university, marriage and parenting as examples. Beyond the arbitrary 65-year-old cut-off point, she adds, people are expected to write the script as they go.
While Canada’s population isn’t aging at the same rate as Japan’s, people here are living longer than ever. In 2023, the average life expectancy was in the low 80s, and it’s been estimated by the Danish Aging Research Center that anyone born in rich nations in the 2000s can expect to see 100. Even today, as the first baby boomers (the second-largest generation, behind millennials) enter their mid-70s, aging is becoming more difficult to ignore. “The social, economic and cultural impacts of this phenomenon are massive,” writes Satya Brink in The Longevity Dividend, a book that examines the potential benefits to society of a longer existence. She adds: “This population structure includes a greater number of adults with knowledge and skills than before that can contribute to society.”
To some extent, this translates into economic potential. The trend of “unretirement” is on the rise, both by necessity and choice. It’s been floated by the World Economic Forum as a possible solution to help mitigate the global shortage of skills. But there’s also a large “grey economy” that is already thriving. It goes largely unnoticed, but many older people take on simultaneous roles as mentors, grandparents and volunteers.

In Canada, older people volunteer more time per person than any other age group. Nearly 40 percent of those aged 55 to 75 take on formal volunteering. For those older than 75, it’s nearly a third. The older group volunteers more than 200 hours a year on average, according to Statistics Canada. Katz reminds me that those figures don’t account for the many hours some grandparents also devote to babysitting and childcare.
When I call Lois Kipfer on a Friday morning, she tells me about her week: on Tuesday, she drove around Stratford, Ont., to deliver Meals on Wheels and worked her regular volunteer cashier shift at a care-home corner store. Next week, she’ll go to her local church to make sandwiches for the unhoused, and on Sunday, she’ll play the organ for service. Lois turned 90 in May and says she’s proud of it.
Of course, it’s not only about what people can contribute physically. In her talk, Grande speaks about moving away from a “settler society built on the exigencies of capital.” By that, she means “the conflation of work with existence, of economic growth with production, of production with wage labour and of old age with declining yield.”
The older generation holds a wealth of knowledge and, given the opportunity, has a lot to teach. With the advent of technology and inexpensive goods, basic skills — like how to can vegetables or sew on a button — fell to the wayside along with valuable lessons for the future. My mother’s parents’ lives were shaped by the Great Depression, when wasting food wasn’t an option. Both were handy around the house. If something broke, they’d fix it. If they could make it themselves, they’d do that, too. In today’s throw-away society, where wasting can feel like second nature, surely our planet could benefit from these perspectives.
Want to read more from Broadview? Consider subscribing to one of our newsletters.
There’s also plenty to be learned from the act of caring itself. On a call, Grande, who was her mother’s caretaker for the better part of a decade, explains that western culture is individualistic: from a young age, we’re taught to celebrate personal achievements over collective ones. We value independence and autonomy. It’s assumed that good things come to those who work hard. “Being in close relationships with older people who often need care reintroduces the notion of care in our daily lives,” she says. “Even in the most challenging times of aging, when somebody’s not well or has dementia or lacks mobility…there’s something to learn from that.” The problem is that there are too few opportunities for these exchanges to take place. By restructuring our cities and care facilities, we could build a much richer and more diverse society.
Again, Japan has lessons. Even outside of Mitsugi, the Japanese town that pioneered the “community-based integrated care” system, the idea that generations can learn from each other is deeply ingrained. At Hotch-no-Lodge, a health clinic and community centre in the town of Karuizawa, residents share their wisdom and skills with the wider community by building relationships with young people through art activities. Japan even has a national holiday called Respect for the Aged Day to honour the contributions the older generation has made to society. On the third Monday of each September, citizens take the day off to spend time with elderly relatives and friends.
The Netherlands also has an innovative approach to caring for its aging population. Its “dementia villages” — gated care facilities that resemble quaint Dutch towns, with cafés, brick townhouses and gardens — are situated within the community at large. And in 2015, a retirement home in the city of Deventer began offering rent-free housing to students as one of several intergenerational housing projects taking place across the country. In a 2019 analysis of the experiment, researchers from the University of Utrecht noted that the retirement home became a central place in the community, hosting everything from billiards matches to college drinking games to photography exhibitions. “As a result, the quality of life and health care has a different dimension: It is experienced and not ‘just’ measured,” the authors wrote.

Some initiatives to bridge the chasms between generations exist in Canada, though not at a national level. In 2000, Sharon MacKenzie, a retired teacher in Vernon, B.C., launched the Meadows School Project as an “intergenerational immersion” program. She set up a makeshift classroom inside an assisted living residence, where a group of students ages nine to 12 would go for eight weeks a year, sharing fitness programs, singalongs, art classes, meals and visits with seniors. Eight years later, she founded the Intergenerational Society of Canada with the goal of broadening intergenerational relations in other parts of the country.
Intergenerational frameworks are starting to trickle into care-home planning, too. Generations Calgary, a complex established by the city’s Ismaili Muslim community, offers independent, supportive living and long-term care units for seniors, but it also includes an early childhood education centre. What started as a pilot project about five years ago has grown into a community space for people of all ages to learn from each other. One resident reads to children three times each week. Some nights, teenagers stop by the complex to play board games with seniors. Families gather outside for lunch. On Halloween, the kids get dressed up and go door to door asking for candy.
“It takes a village to raise a child, but it also takes a village to care for its elders,” says Safiqa Kara, the centre’s director of care. “What we’ve created is a sense of community where our elders are perceived not as expensive burdens, but as valuable members with important lessons to teach.”
In the next few years, Kara says Generations plans to open four additional locations: two in British Columbia, one in Laval, Que., and another in Toronto. “We’re early in the stages of these models,” says Kara. “But I can’t wait for the day when this is just a part of care.”
***
When I spoke with MacKenzie of the Intergenerational Society of Canada, she told me an old folktale about a king who wanted to get rid of all the old people in his village. Young people, he proclaimed, looked nicer and were more productive. When a little boy caught wind of this, he ran off to his grandfather and told him to go hide away in the mountains to save his life. The boy continued to care for his grandfather, bringing him food every day.
Years passed in the seemingly happy village before a plague swept through, felling villagers with a terrible sickness. The same problem had happened years before, and the inhabitants had been able to survive it. But since they had gotten rid of everyone who lived through it, they were at a loss to know what to do.
The king proclaimed that anyone who could offer a solution would become rich and take over the kingdom. Of course, the grandfather held the answers the king was looking for and his insight saved the lives of many.
The story still feels relevant today. We may not toss away our older people in a literal sense, but in many ways we do exile them. If we slowed down and took a moment to listen to them, perhaps our society, too, could become wiser for it.
***
Albert Kniesz died a few weeks after this story was written, on Oct. 12, 2023, at age 92. He was the faithful husband for more than 67 years of the late Beatrice Kniesz, who died in December 2022, the devoted father of three daughters and the beloved grandfather of seven grandkids.
This article will appear in Broadview’s January/February 2024 issue with the title “Seniors’ Moment.”
We hope you found this Broadview article engaging.
Our team is working hard to bring you more independent, award-winning journalism. But Broadview is a nonprofit and these are tough times for magazines. Please consider supporting our work. There are a number of ways to do so:
- Subscribe to our magazine and you’ll receive intelligent, timely stories and perspectives delivered to your home 8 times a year.
- Donate to our Friends Fund.
- Give the gift of Broadview to someone special in your life and make a difference!
Thank you for being such wonderful readers.
Jocelyn Bell
Editor/Publisher