When Megan Rolfe was 18 and in her first year of college in London, Ont., her struggles with depression took a sharp turn, and she found herself gripped by suicidal thoughts. After attempts at taking her life in both 2012 and 2013, she packed up her bags and went home to her family. But she didn’t seek out a therapist.
Instead, Rolfe threw herself into work, hoping the distraction might help alleviate some of her symptoms. “I didn’t want to be the only one of my friends who was going to therapy,” says Rolfe. “I thought maybe it was something that time could change.”
You may unsubscribe from any of our newsletters at any time.
A few years later, Rolfe got a job in hospitality and moved out to Lake Louise, Alta., where she fell in love with the mountains and came to view spending time in nature, and specifically hiking, as a form of therapy. Still, she continued to struggle with her mental health — and was now far away from family support — so she started to look for help.
Tiny Lake Louise, where the wintertime population can shrink to just 500, has one psychologist accessible through the public health-care system. When Rolfe called his office, she was told she’d have to wait several weeks for an appointment. When she finally got one, she was prescribed anti-depressant and anti-anxiety medications. But the psychologist could only meet with Rolfe every couple of months after that, and private care in nearby Canmore, Alta., was prohibitively expensive. “I didn’t know what I was looking for,” Rolfe says. “[Therapy wasn’t accessible], so I just put it on the back burner.”
Later, Rolfe moved to Canmore, where she decided to wean herself off her medications. Then, two months later, she was out hiking and suddenly became disoriented. She walked right off a ledge and fell nearly two metres, narrowly escaping serious injury. “I couldn’t see straight, I was crying and nothing was going on that caused it,” says Rolfe. “It was a massive panic attack at the top of a mountain. That’s when I realized I needed to see somebody.” But with a net monthly income of about $2,800, it was hard to afford the help she required.
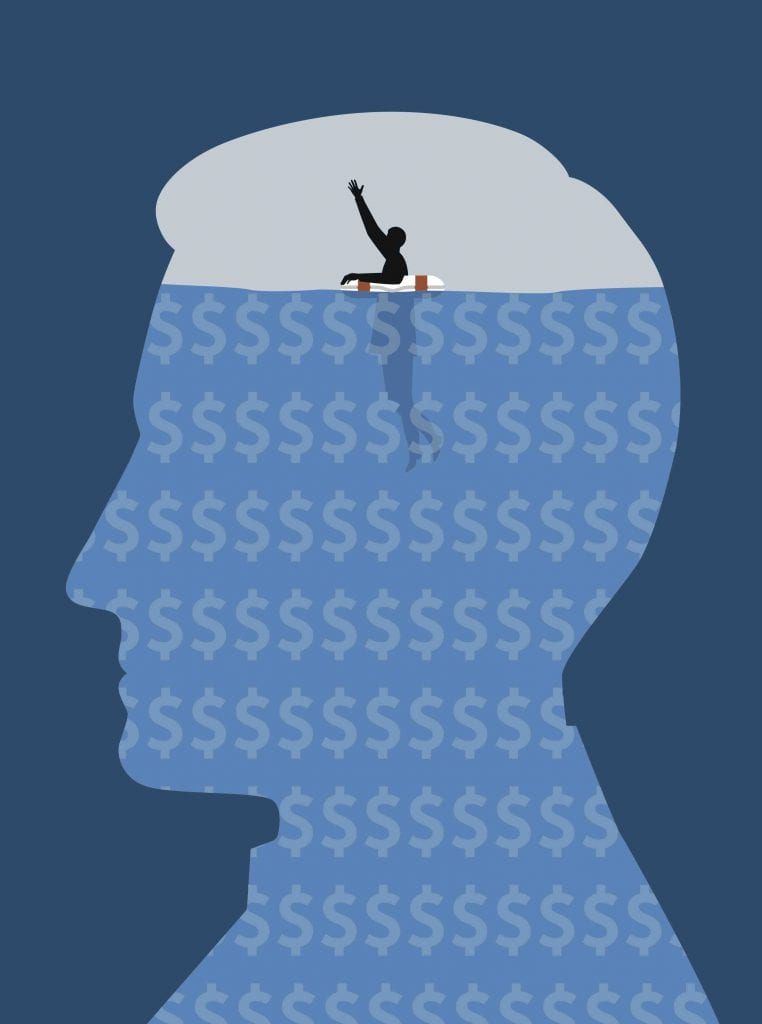
Rolfe is just one of 6.7 million Canadians who struggle with mental health, many of whom are unable to access affordable and timely mental health-care options. Levels of care across the country are inconsistent because therapy and other forms of mental health-care treatment are delivered and largely funded by the provinces and territories. The resources that do exist are lacking, which too often means people have to reach desperate lows, possibly even suicide attempts, before they can access public care.
After her scare on the mountain ledge, Rolfe called her parents, who agreed to pay for private therapy: $140 per 50-minute session. Now 25, she has a job that offers benefits, but the $350 per year allotted to counselling doesn’t go very far. “Depending on how severe your mental health is, you could go through that in a month,” she says.
Rolfe isn’t alone. According to a 2018 survey conducted by the Canadian Mental Health Association (CMHA), 85 percent of Canadians say that mental health services are among the most inadequately funded aspect of health care. The Mental Health Commission of Canada (MHCC) estimates that 50 percent of Canadians will have or have had some form of mental illness — anything from schizophrenia to an anxiety disorder — by the age of 40. However, in 2015 governments dedicated only 7.2 percent of health-care funding to mental health.
This funding gap means that a large group of Canadians go without adequate care. In 2017, the MHCC said that “statistics bear out the existence of widespread, and at times acute, unmet need.” Approximately 80 percent of consultations with psychologists in Canada take place in the private system, meaning Canadians without insurance — and even some who have it — are paying out-of-pocket for services.
The situation is particularly dire for young people. Children’s Mental Health Ontario found that children and youth in urgent need of mental health care are waiting up to one and a half years for treatment in some parts of the province. Across the country, the second leading cause of death among children is suicide.
“An alarm bell needs to be rung,” Sara Austin, founder of Children First Canada, told Global News following the organization’s release of a 2018 report on the mental and physical health of children. “There are a range of factors [that contribute to mental health issues]. Our report also highlights the number of kids who experience child abuse — one in three in Canada. That’s also closely linked to mental health outcomes.”
As it turns out, little has changed over the years when it comes to Canada’s mental heath-care funding. Today’s headlines are full of warnings about family physician shortages and cuts to health-care budgets, but Erika Dyck, Canada Research Chair in the History of Medicine at the University of Saskatchewan, says that mental health services have always been underfunded. She points out that funding has actually diminished since we moved away from large-scale, residential mental health facilities to community-based care by the 1970s.
At that time, the programs previously delivered in a residential setting were largely converted into outpatient programs, with many psychologists treating patients in hospitals. But waves of health-care defunding — in Ontario, for example, former premier Mike Harris drove deep cuts to health-care spending in the 1990s — forced many psychologists into private practice, leaving prospective patients scrambling to find affordable care.
“When it splinters into different jurisdictions, it becomes notoriously difficult to determine how much funding is really earmarked for mental health care,” says Dyck. “And even when you add up all of the pieces, there’s still a steady decline or defunding of mental health services.”
“An alarm bell needs to be rung.”
Sara Austin, founder of Children First Canada
Many experts believe a big issue behind the lack of government funding is the question of whether we view these services as an essential part of holistic health. “You hear ‘man up’ a lot,” says Sylvain Roy, a neuropsychologist at the Centre for Addiction and Mental Health (CAMH). “The idea that you don’t need to talk to anybody [and] it’s all in your head. This perspective is still really out there, even among the bureaucrats in the Ministry of Health.…If we don’t address that, we’re going uphill trying to solve the problem.”
There is still a lot of stigma and shame around mental illness, too. According to CAMH, in 2008 42 percent of Canadians were uncertain if they would socialize with a friend who has a mental illness, and only 50 percent would tell friends or co-workers that they have a family member with a mental illness (compared to 72 percent who would discuss a diagnosis of cancer). Megan Rolfe says the stigma caused her to hesitate to contact a therapist before her panic attack on a mountain in Alberta. “People can say that you should reach out if you’re struggling, but it’s still embarrassing,” she says.
Thankfully, mental health treatment is being talked about more openly than ever before, and depictions of care are all over the media. Talk therapy, for example, has become a clear part of the zeitgeist, with patient-therapist relationships captured on everything from Big Little Lies to HBO’s In Treatment. Even Colton Underwood of The Bachelor talks openly about his therapy. In Canada, mass-media campaigns like #BellLetsTalk help to break down stereotypes and encourage people to ask for support.
This type of exposure could have a positive impact in terms of awareness. A 2014 study led by McMaster University in Hamilton found that there has been a threefold increase in the number of people who say they need help since 1983. Yet the already-burdened public system struggles to respond. Funding has not materialized to address the growing need, leaving resources stretched and typically reserved for the most acute and serious cases. “We’re seeing more ER, hospital and physician usage,” says Roy of CAMH. “The public system is simply not equipped to deal with the demand.”
Jen*, who is raising two children in Toronto, has been frustrated by the lack of access to preventative care. She’s a single mother who mostly works as a freelance writer and magazine editor, and she has money for housing, food and clothes. But private psychological services have been largely inaccessible.
Jen’s son, now 24, has consistently struggled to access psychological services through the public system even as he has been diagnosed with learning disabilities, anxiety and depression. When he developed severe social anxiety in his mid-teens, he sat on a waiting list for funded cognitive behavioral therapy for about 19 months.
Knowing her son was struggling but not able to access help, Jen was left feeling sad, desperate, isolated and angry. “I wondered what kind of system could allow a teenage boy who has the courage to ask for help to wait more than a year and a half without professional assistance,” she says.
Her 17-year-old daughter also has mental health diagnoses, but a suicide attempt years ago seemingly bumped her up the chain of priority care. “It’s really tragic that children, who could be helped when they’re in the early stages of depression and anxiety, have to let things slip to the point where there’s self-harm or harm of others,” reflects Jen.
Recent studies prove Jen’s experience isn’t uncommon. According to 2014 data from McMaster University, only one third of young people in Ontario with a mental health disorder had seen a specialized professional in the last six months, which study authors largely blamed on gaps in public mental health services.
Adults, too, struggle with access. According to 2012 data from Statistics Canada, one third of Canadians 15 and older reported that their mental health-care needs had not been fully met. With few options for preventative care, up to 80 percent of Canadians rely on family physicians for mental health care. We also spend close to a billion dollars — a third out of pocket — on counselling services every year.
The long-term impact of lack of care can be catastrophic and sometimes fatal. Poverty and mental health issues are inextricably linked. According to the CMHA, more than 70 percent of Canadians with a serious mental illness are unemployed, and those living below the poverty line experience the highest number of chronic disorders.
“The people who experience poverty and homelessness tend to be the ones who need these services the most, and they’re least likely to have access,” says neuropsychologist Roy. “With poverty comes limited ability to secure housing, being able to pay for basics like food and clothing.…[People] get stressed out and unable to cope. We’re not giving people the ability to get out of that and overcome it.”
“I wondered what kind of system could allow a teenage boy who has the courage to ask for help to wait more than a year and a half without professional assistance.”
Jen*
Several provinces have announced funding increases in recent budgets, and in 2017 the federal government announced an additional $5 billion in spending earmarked specifically for mental health services to be rolled out over 10 years. But after the federal announcement, Chris Summerville, then-co-chair of the Canadian Alliance on Mental Illness and Mental Health, told This magazine the funding was a “mere drop in the bucket to address all the lack of resources and capacity.”
While the CMHA praised the federal funding as “a great start” in a press release, it called for “continued investment in mental health — especially in community-based services and support — to bring Canada in line with other G8 countries, where it still lags behind.”
And so, with a public system stretched to the brink and a private system that’s out of reach for many people, new, creative solutions are helping bridge the gap. Strongest Families, for example, a project in Nova Scotia based on a six-year research program by the IWK Health Centre, makes use of phone and internet technology to offer free mental health coaching for families with children between the ages of three and 17. Last year, Strongest Families had over 6,000 referrals, and the organization expects that number to rise to 7,000 in 2019. This is a way to help avoid long wait-lists and spare parents the financial burden of travel and taking time off work to consult mental health professionals.
Other online tools are also being promoted as a possible lower-cost, accessible mental health-care option. Montreal’s mind.me app, for example, can help diagnose, manage and predict depression. Inkblot and Hasu, startups launched in Toronto in 2015 and 2016 respectively, offer affordable virtual counselling for clients across Canada.
One Toronto-based startup, TranQool, remotely connects people to video therapy. Saeed Zeinali says that he and his co-founders started the business because they found mental health-care services lacking even for young professionals. “There was a wait time, it was expensive and you had to travel,” he says. “You couldn’t have access to it when you needed it.” (TranQool was acquired by HumanaCare, an employee health service provider, in 2018.)
For people more comfortable with in-person options, low-cost, sliding scale or even student-delivered counselling options have popped up across the country. One private clinic in Vancouver maintains a network of free or low-cost counselling options, often offered by graduate-level psychology students. This is part of a compassionate resistance movement to challenge long public wait-lists and help those with limited discretionary income.
Rolfe, who struggled to seek out professional help, first because of the stigma and then because of the wait time and expense, has stabilized since she started seeing a therapist. But while she feels stronger and happier in her mountain home, she also has an enduring sense of how close she came to catastrophe.
“My therapist has been like the light at the end of the tunnel,” she says. “Having someone to talk to that just listens to me and allows me to work through my problems, and helps me understand how my brain works…allows me to see myself in a new light.”
Rolfe’s close call has given her the courage to speak out about much-needed reforms in the Canadian system. There’s no doubt that public mental health care in Canada requires greater funding, and that funding is tied to compassion and how we prioritize the needs of vulnerable people in society. To combat stigma, Rolfe believes mental health-related information needs to be a core part of early education, especially since many disorders first appear in childhood. And she sees affordability as a key part of accessibility.
“I hope that one day we can see all mental health services included in our Canadian health care, or that schools and workplaces offer free services,” she says. “People and families with lower incomes should have the same access to mental health services that middle- and upper-class people do.…In an ideal world, all therapy is free.”
*Name has been changed
This story first appeared in Broadview’s December 2019 issue with the title “Out of reach.”









This article motivated me to change the fee structure of my private practice. I am providing Therapy-Geared-To-Income for modest income workers. Visit my website at suelamwellness.wixsite.com/home
I have great empathy for those suffering from mental health conditions. My own biological mother (I was adopted at 2.5 months) had serious mental health issues and was in and out of institutions her whole life. I’m also prone to minor irritation from mental health conditions which I suspect was a biological condition at least as far back as my maternal great-grandmother.
My wife is a psychotherapist that has seen a disturbing rise of mental health related conditions over the last 10 years that contribute to many major individual and family issues. Although I suspect there are many contributing factors, one that I’m particularly concerned about is how technology enables business and society to move at an ever more frantic pace. Any casual reading of the academic and popular literature indicates that this is contributing to continual major stress on our modern society and especially on our most vulnerable. I’m interested in this issue because for over 20 years, I was at the forefront of the IT Tech revolution – as a technical analyst, manager and consultant.
I fear that technology is like a run away train (to coin a phrase by Ronald Wright) that is contributing to us headed for the edge of a very large cliff. If we don’t start to seriously ask questions as a species – such as whether all this rapid technological development is warranted given how it enables society and business to change so quickly and produce so much “stuff”, we may go over the cliff. Technology significantly effects everything from mental health to the environment – and some of our wisest modern prophets, such as Ronald Wright and Derrick Jensen, think we are in for a very rough ride that will make Covid seem like a walk in the park. I find it ironic that a technology company, Bell, is sponsoring mental health day. .
My first call to make an appointment for therapy resulted in chastisement for not having a credit card and for wanting to pay cash. Told me no one would accept me without one and when my ADHD got the better of me and forgot to respond to an email I was dropped before my first session. Went the entire pandemic alone in my house for 2 years. Now I’m trying again and have just been so defeated by my last attempt and now things are even more dire as it got so bad I quit my job out of panic and lost my house and it seems like with everything else going on with the mental health care industry I’m starting to see that there is only 1 real solution. This article kind of confirms my morbid rationality.