In April 2020, my mother and I walked through our neighbourhood to put up a dozen cross-stitched messages that she had been working on since the pandemic began. It was early spring in Winnipeg, where people were taking to the streets en masse to shake off their pandemic doldrums despite the chilly weather. We stapled the cross-stitches to wooden utility poles along the sidewalk, in full view of passersby. They carried simple messages: “Take care,” “Alone together,” “Hang in there” and “You got this!”
During those early days, nearly everyone seemed to be struggling. I listened to podcast episodes and read think pieces about how we were all in a state of collective mourning for the “time before.” The cross-stitch messages were meant to be small reminders to our neighbours to look after each other as they grappled with new feelings of anxiety and hopelessness in the face of a looming tragedy.
You may unsubscribe from any of our newsletters at any time.
For my mother and me, the messages were also an extension of what we had been telling each other. We both live with mental illness, and for the past year and a half we have been talking nearly every day about the ways anxiety and depression affect our lives. We share tips to deal with panic attacks, encourage each other to meditate or do yoga, and compare our experiences with therapists and anti-depressants.
My struggles with mental health predate the pandemic, and for the longest time I didn’t even register that I was sick. Other people in my life had mental illness — friends, lovers and family members — and I thought mental illness was for them. I felt like I wasn’t anxious enough or depressed enough to be mentally ill. For years, it was like a constant stomachache or a sore knee — nothing debilitating, but it wears you down over time.
It wasn’t until my illness began interfering with my work that I took it more seriously. I was a year out of university and had recently left a well-paying job to start freelancing. During that period, there were weeks when just getting out of bed and completing a simple task, such as responding to an email, felt like an enormous effort. My rapidly filling inbox would pluck at my anxiety, until I felt it was fruitless to even begin tackling the mountain of work that had built up. I would feel a deep, unshakable shame at the end of a day when I had accomplished nothing.
Somehow, I would still get everything done — because I always did — but it would be at the expense of sleep and with the help of my then-boyfriend’s Ritalin, which kept me awake and focused into the early hours of the morning when I was staring down a deadline. Near the end of my relationship with that boyfriend, when things were getting particularly messy, I finally started seeing a counsellor. It was a revelation for me when they confirmed in our first meeting what I already knew to be true — that I had depression and anxiety.
Since that session, I have reflected on the origins of my mental illness. Sometimes, that has meant literally looking into a mirror. I have my mother’s hair and my father’s nose. I haven’t done a side-by-side comparison of our ears, eyes and mouths, but I’m sure there would be plenty of similarities there, too. But what about the parts of us that lie beneath the surface of our skin? What about my stresses and anxieties, my fears and sorrows? Where do they come from? While it may be easier to attribute depression or anxiety to a chemical imbalance in the brain coupled with the stresses of work or a bad breakup, I wondered if there was a deeper explanation.
More on Broadview:
- Why it’s so hard to find affordable mental health care
- How to take care of your mental health this winter
- When kids are in crisis, how can we help them?
According to the Maryland-based National Institute of Mental Health, mental disorders can be caused by biological, environmental, psychological and genetic factors. The organization even says that one’s family history may be the best way of determining one’s risk of developing mental illness. In 2013, the Lancet reported that two specific gene variations have been found to correlate with five different mental disorders, from major depression to autism.
However, it’s not as simple as saying that everyone with these genetic variations will develop mental disorders. Although he maintains that the findings are statistically significant, the study’s co-author, Dr. Jordan Smoller of the Massachusetts General Hospital, admits that these genetic associations “can only account for a small amount of risk for mental illness.”
These were the kinds of insights I was looking for when, shortly before COVID-19 sent the world spiralling, I moved back in with my mother for the first time in nearly six years. I had just ended the longest relationship of my two-and-a-half decades of life, and she was dealing with a host of work and life-related stresses. We were both near our mental health low points, finding it hard to take on much beyond the bare minimum, and we were leaning on each other for support. I began to wonder whether our experiences with mental illness could somehow be connected.
My mother describes herself as an intense child who was invariably fraught with anxieties. She has a clear memory of lying in bed at around age 11, marvelling at the fact that, for once, she didn’t feel stressed in that moment. Other nights, she would lie awake for hours, going over her memories of school, swim practice, interactions with friends and other things she worried about as a Grade 6 student. “I always felt everything very deeply,” she tells me.
Years later, when she was in her early 20s, she had her first major panic attack while participating in a Canada World Youth volunteer program. It had been a busy and sometimes stressful summer for her. After working at a café in southern Germany for part of the summer, she and my father travelled around Europe before returning to Canada. She had just a few days at home before jetting off again, this time to Quebec, where she was immersed in a French-language community.
Toward the end of the summer, during a dinner at a restaurant outside Montreal, she fled from the group, seemingly without reason. More than three decades later, that whole night is still a blank spot in her memory — she doesn’t recall anything between the dinner and, sometime later, crouching in the dark in a bush next to the road, not sure where she was. She only knows she was trying to get to the airport and home to Alberta.

She still has panic attacks, although they’re less debilitating now. She recognizes the symptoms, such as a racing heart rate, an inability to catch her breath and a narrowing of her vision — and understands that no, she’s not having a heart attack. She’s learned how to slowly bring herself out of these incidents. Sometimes that looks like lying on the floor under her desk, while other times it means doing breathing exercises or going for a long walk outside.
I have also felt that rising panic in my chest, the shortness of breath and the tears welling up behind my eyes. When I was younger, these emotions came out as bursts of anger or frustration, often misdirected at friends, teachers and other authority figures. As I’ve grown older and learned to curb these outbursts, they emerge in other ways, as uncontrollable sobs, seemingly out of the blue, when I’m on the bus or on my lunch break.
I asked my mother if she recognized her struggles with anxiety in me. “Right from the time you were born I would look at your face and I would see my own,” she says. “Naturally, I would feel worried when you were feeling deeply about things.”
***
Jehannine Austin has been interested in the potential connections between mental illness and genetics for most of her professional life. She’s a professor in the University of British Columbia’s department of psychiatry and medical genetics, and in 2012 established the world’s first psychiatric genetic counselling clinic in Vancouver. Since then, psychiatric genetic counselling clinics have popped up around the world. In these clinics, counsellors help people trace a detailed family history of mental health and then work through connections between this history and their own mental illnesses.
“I have a history of depression myself, and I live with anxiety,” says Austin. “So this is all very personal stuff for me.”
When Austin became interested in using genetic counselling to work with people living with mental illness nearly two decades ago, she says there was initially some push-back. “Nobody would hire me to do it,” she says, adding that at the time there was no evidence it could be helpful or that people with mental illness would even want genetic counselling. That’s how she fell into a career as a researcher, so she could determine whether learning about the genetics of people living with conditions such as anxiety, depression, bipolar disorder and schizophrenia could help them receive better care.
She found that many people with mental illness were searching for answers to explain why they feel the way they do. Without answers, she says, people often experience guilt and shame. They load the responsibility for their illness onto themselves, feeling like it’s somehow their fault that they are depressed or anxious. The questions she tackles with people in her sessions include: Why me? Was there something I did that caused this? Is there hope for me to be better in the future? “It’s really an existential thing,” she says about the counselling process.
The answers aren’t exactly clear, though. A number of studies on the connection between mental health and genetics have been conducted over the past decade, and the insights are complicated.“The result is a mess,” wrote Michael Marshall just last year in Nature about the diverse findings of these studies. Instead of direct connections between our genetics and our mental health, Marshall writes that “hundreds of genes each have a small effect.”
“I have also felt that rising panic in my chest, the shortness of breath and the tears welling up behind my eyes. When I was younger, these emotions came out as bursts of anger or frustration, often misdirected at friends, teachers and other authority figures.”
Austin uses similar language. She doesn’t believe people directly inherit mental illness from their parents, but that they instead inherit “genetic vulnerabilities” to mental illness. Austin uses a metaphor she calls the “mental illness jar.” Each of us is born with our jar filled to a certain level — these are our inherited genetic vulnerabilities — and we are stuck with this much in our jar throughout our lives. However, as we grow and experience life, our circumstances can add to the jar. A period of intense stress or a death in the family, for example, could contribute to our jar, and if the jar becomes filled to the top we have an episode of mental illness. Some people’s jars may never reach that point of overflowing. This may be because they were born with fewer genetic vulnerabilities, or it may be because they experienced fewer life challenges.
When I asked my mother about the possibility of inheriting a genetic vulnerability for mental illness, it seemed like something clicked. The idea resonated with both of us. I have been thinking about the ways my experiences with depression and anxiety reflect my mother’s, and as my mother has been working through her mental illness, she’s been thinking a lot about her grandmother Elfriede Würmann. “The image I have of her is that she was never happy,” my mother tells me.
Elfriede was born in 1915 in Germany and raised two sons, including my grandfather, during the Second World War while her husband was away fighting on Crete. After the war ended, her husband was captured and held in a prisoner-of-war camp in Yugoslavia, and for years she assumed he was dead.
Many people in my family speak about Elfriede being depressed in the later years of her life, describing her long face and dampened spirit. After her husband had a stroke in the 1980s, she went to a doctor to tell him about the way she was feeling. Instead of helping her, the doctor asked, “Who is the one who is sick? Is it you or your husband?” She stopped seeking help for her depression after that.
My grandfather was convinced that his mother’s depression began with his father’s stroke. “Up to that point, my mother could handle life,” he said. “Suddenly, she couldn’t, because she couldn’t do anything about my dad.” But I can’t help but wonder if it’s more complicated than that. I think about what Austin told me about the genetic vulnerabilities we all inherit, and I find it hard to believe that Elfriede’s depression suddenly appeared in her 60s.
More on Broadview:
- More older women are drinking too much. A new sobriety movement aims to help.
- Portraits of students’ mental health: “We are not broken”
- Agoraphobia closes doors for sufferers during the COVID-19 pandemic
In recent years, research has been conducted into the idea of inherited family trauma, especially in relation to descendants of survivors of the Holocaust or Indian residential schools. While these are extreme examples of a traumatic event that can affect generations, further research also suggests that inherited trauma can affect anyone. “Many of us walk around with trauma symptoms we can’t explain,” said Mark Wolynn, author of It Didn’t Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle, in an interview with Psychology Today. “We might have a life-long depression that feels like ours but isn’t ours.”
According to Wolynn, mental illness symptoms could be the result of trauma that has been inherited. “One of the most obvious signs is that we can experience a sudden onset of anxiety or fear when we hit a certain age or reach a certain milestone,” he says. “It’s as though there’s an ancestral alarm clock inside us that starts ringing.”
To explore my own history, I wanted to learn more about Elfriede. So I visited my grandfather in his 24th-floor apartment in the middle of the pandemic summer. We sat a couple of metres apart; I wore a mask, and I sanitized my equipment before pushing record. My grandfather’s apartment overlooked Winnipeg’s sprawling urban elm forest. It all seemed so far removed from the stories he was telling me.
During the war, Elfriede and her sons moved out of the city to avoid the bombings and lived with their relatives on a farm. She worked as a seamstress, trading her labour for food and other necessities. Despite the challenges, my grandfather said his mother was a joyful person during this time. “We were always singing when we did the dishes,” he said, adding that Elfriede was “always whistling and full of vigour.”
However, just because Elfriede sang and whistled doesn’t mean there wasn’t sadness or worry around their house. “There were sad times,” he admitted. In his family, it was acknowledged that this was a part of life, and he recalled his mother joking to “enjoy” being sad. “You don’t have to be strong when you’re sad,” she would tell him. “If you need to cry, just go ahead and cry.”
Talking with my grandfather about mental illness, I sometimes felt as though we were communicating across a great divide. He spoke in terms of clear causes and effects. I asked him if he had ever felt depressed or anxious, and he described a time in his early 30s, when he and my grandmother were living in Whitehorse with four children under the age of six. He hesitated to use the word “anxiety” but told me that there were times at the end of the month when the young couple could barely afford groceries. “There was a reason for me being anxious, and I think if you’re anxious for a reason, you should be.”
“One of the most obvious signs is that we can experience a sudden onset of anxiety or fear when we hit a certain age or reach a certain milestone. It’s as though there’s an ancestral alarm clock inside us that starts ringing.”
But it’s not always that cut and dried for me. Often, I have a hard time determining what is causing my anxiety, or why some days I wake up feeling depressed and others I wake up feeling fine. I think about my unexplained anxieties or depression and I wonder if these could somehow be connected to a trauma experienced by Elfriede or one of my other ancestors whose experience of mental illness I know less about.
Of course, one of the main reasons for learning about these family histories is to also figure out ways to make mental illness a less disruptive part of one’s life. Although our genetics or inherited trauma may predispose us to have a full “mental illness jar,” as Austin puts it, she also emphasizes that there are ways to manage its contents. Strategies such as exercise, routines, healthy eating habits, a good night’s sleep or the right medication can help people avoid reaching the point where their jar is overflowing.
Just a couple of years ago, my mother began cross-stitching to help increase the size of her own jar. Most of the pieces she’s stitched have a minimalist style — colourful text on a plain background. She’s referred to it as a form of meditation, a way to ruminate on a particular word or phrase as she pierces the fabric with the needle and draws the thread through, over and over, until it’s finished. She’s stitched simple words, such as “love” or “peace,” as well as profanity-laced slogans such as “fuck the patriarchy.”
She stitched a series of pieces at the beginning of the pandemic, the ones that I described at the start of this essay. In the weeks after we stapled the messages to the utility poles around our neighbourhood, we watched as people shared their discoveries of the cross-stitches on local Facebook pages, describing how they had brightened their day or reminded them of the good in the world.
It’s been more than a year since then, and, on the whole, I think I can confidently say that my mental health has improved. My mother and I still talk about the ways we experience our mental illness and the coping mechanisms that we have developed, but these days our conversations are less about managing mental health crises and more about whether we are feeling well enough to slowly wean ourselves off our medications. At the same time, I am now aware of the family history of mental illness that will shadow me throughout my life, possibly stitched into my very DNA, and how I’m more prepared than ever to take it on.
***
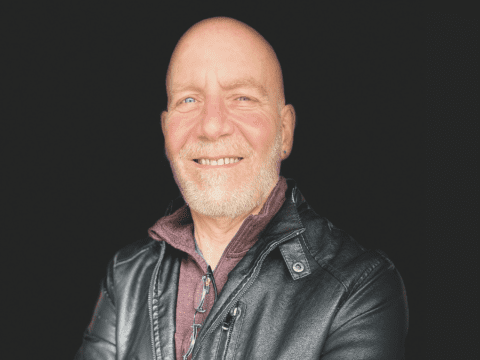
Isaac Würmann is a writer based in Berlin.
This story first appeared in Broadview’s Oct/Nov 2021 issue with the title “My father’s nose, my mother’s anxiety.”










Really appreciate the two articles I read about mental illness. Various in my family. Always good to read more about it. Great magazine. We support you.
My mom has a mental illness and it makes her believe she’s seeing bugs and parasites. When she’s not seeing anything at all.