Story translated by Brigitte Gemme
“You are Ms…?” For the fifth time in as many minutes, I recite my name, date of birth and the reason I’m there to yet another masked person. Success! My nervousness hasn’t made me forget my identity.
You may unsubscribe from any of our newsletters at any time.
As the hospital staffperson puts papers back in a binder, she asks, “Would it be nosy to ask you if you are doing this for someone you know?” No, not at all. I know nothing of the receiver. All I know is that they are getting a new kidney today.
The anesthesiologist joins us. She asks me to identify myself (sixth time!) and if I suffer from motion sickness. I think hard about the right answer, mindful of being precise: “Not really, but maybe a little bit.”
That seems to satisfy her. She gives me some instructions and invites me to enter an operating room of the Centre hospitalier de l’Université de Montréal (CHUM).
So far, I have been lying down on a rolling bed, as if I am sick. But I am in great shape. The day before, I beat a personal record — and lots of guys — on my bike on Zwift (an indoor cycling app). Those last few steps separating me from the operating room are the last ones I will take with my two kidneys. “Can I walk in?” Of course, no problem.
The room is nothing special. Kind of small, well lit. There are screens and instruments. In the middle, a narrow table with two outstretched armrests that form a cross. I can’t help but think of execution tables but swat away that creepy thought. At the request of the medical personnel, I lie down on my back. It is really uncomfortable, like lying on a wooden board. But it is my choice, and I have clearly expressed my consent. I am about to give a kidney to a stranger.
Dialysis or transplant
“Ms. Desaulniers, time to wake up.” Like every time someone calls me Ms. Desaulniers, I think about my mother. Then I settle back into reality: the operation is complete. I am well. What exactly happened? The anesthetics have taken a chunk of my memory.
Later, I find a selfie on my phone. I look stoned, with oxygen up my nose. At least I had not posted it on Instagram. Late in the afternoon, the doctor frees me of my remaining worries. The recipient’s surgery has also gone well.
Little in my life predestined me to donate a kidney. As a child, I wanted to become a nurse. I tended to my dolls’ health with a Fisher-Price medical kit. My interest in human health faltered when, accompanying my father to a blood donation drive, I found out that needles made me faint. I never watched medical TV shows, nor was I ever close to a sick person. As an adult, I only went to the hospital once, in college, after fainting in the bathroom of a Trois-Rivières bar.
My knowledge of organ transplant and health in general was fairly limited when I sent my first email to the CHUM organ transplant team, asking whether I could donate anonymously. I vaguely knew that most transplant organs come from deceased donors. I had randomly heard about live donations and thought I would inquire.
Fifteen years earlier, some colleagues had told me that our company’s disability insurance plan had declined the claim of a co-worker from our Toronto office who had donated a kidney. How did they justify the refusal? The surgery had been voluntary. If the insurer paid for this man’s disability claim, they would have to pay for everyone. We chuckled. As if everyone was going to start giving kidneys to strangers. You’d have to be a bit cuckoo to do such a thing, no?
A few months earlier, if asked where my kidneys were, I would probably have pointed to the cavity above my buttocks — and been laughed at. Kidneys are in fact higher, in the back of the abdomen, sitting just below our ribcage, separated by our spine.
My cat Souzex had died the previous spring from kidney failure, like so many senior cats. I saw her slowly lose interest in everything, even wet food, and collapse. Her passing gave me cause to learn about renal function. Kidneys are only about four centimetres long in cats, around 12 in humans, and are shaped like, well, kidney beans. They regulate the amount of water and minerals in the body and eliminate waste, excess fluid and toxins. Kidneys also secrete hormones that regulate blood pressure, produce red blood cells and maintain blood calcium levels. When the kidneys break down, it’s game over: the body fills up with substances that the kidneys were supposed to filter out. Surgeons like to remind people that “the stupidest kidney is smarter than the smartest doctor.”
In humans, kidney disease is common. One in 10 people in Canada suffers from it. There are many causes, including diabetes, high blood pressure, hereditary factors, infections and pharmacological interactions. Those suffering from systemic inequalities, like sexism, racism and classism, are disproportionately affected.

As I found out with Souzex, kidney failure is usually irreversible. When kidneys can no longer perform their essential work, there are only two options: dialysis or transplant.
Hemodialysis patients stay connected for hours, multiple times per week, to blood-filtering machines. Their daily lives are impacted and their life expectancy plummets: only four in 10 people on hemodialysis are still alive five years after the start of the intervention.
Transplant is the other option. When the graft organ comes from a deceased donor, the survival rate after five years is over 80 percent. The new kidney is tolerated by the body for nine years on average. After that, another transplant is possible. When the graft organ comes from a live donor, the survival rate after five years approaches 90 percent and the organ remains functional for 15 to 20 years.
From a financial point of view, governments benefit from promoting transplants. A 2011 study by the Canadian Institute for Health Information found dialysis costs $60,000 per year per patient, whereas a kidney transplant only costs $23,000 plus about $6,000 per year for anti-rejection drugs. Transplants save the government $250,000 per person in a five-year period.
However, supply is dwarfed by demand. Adult patients have to wait on average four years before getting a cadaveric transplant. Those who can find a living donor wait far less (18 months), as the organ usually comes from a relative or friend. Currently, living donations account for only about 26 percent of transplants in Canada.
What if I could save a life?
Ignoring the experience of those living with chronic disease is easy. Their suffering is often invisible. I spent most of my life not even thinking about it until April 2021, when the Facebook algorithm (between excessively long status updates, sourdough bread pictures and posts railing against public health orders) showed me the call for help of a man who needed a kidney.
I instantly connected the dots. My 40-something body could save a life. I typed “kidney donation” into Google and found many websites from 20 years ago featuring PDF forms you couldn’t type into. It all seemed complicated. I was not interested in giving to a specific person. I did not want the recipient to feel like they owed me. I wanted to donate anonymously.
The official paperwork first led me to believe that it would not be possible. Every document mentioned relatives and friends. But, finally, I found this short paragraph at the bottom of a long page on a government site: “The donor can also not be connected to the recipient and decide to donate a kidney. The kidney is then transplanted to a person awaiting an organ who is unknown to the donor.” Bingo.
Over the course of the following months, I had dozens of conversations with the nurse from the transplant centre and submitted myself to many tests. I had blood drawn so many times that I no longer teetered on the edge of fainting when it happened. I collected my urine for 24 hours in a lovely orange jerrycan I had to keep in the fridge. (That day, I worked from home.) My body was scanned and X-rayed, my blood pressure monitored, my breasts squished for a mammogram and my soul scrutinized by a social worker, a psychologist and a surgeon.
I knew I could withdraw my consent at any moment. But moving forward through the process only increased my resolve. I now had a goal. My body could save a life.
The first time we met, the nephrologist (kidney specialist) drew a nice graph for me. He expertly sketched it upside down so he didn’t have to turn the sheet. After turning 40, we lose about one percent of our kidney function every year. Taking out one kidney means that the other one works a little harder. Two months after the procedure, I would still have a little less than 75 percent of my renal capacity.
With a balanced lifestyle, I could stay in good health for a long time. Nothing exotic: exercise regularly, eat well, avoid smoking, watch out for urinary infections, see my family doctor every year and opt for Tylenol rather than Advil. (I always preferred Advil — maybe it was the branding — but I was ready to change my ways.)
What about the dangers of the surgery itself? When I asked, the doctor pulled up a sombre PowerPoint slide. The data compared the risk of kidney donations to that of other procedures. Obviously, I wasn’t the first person to ask. The nerd in me had to take a picture of the screen.
In humans, kidney disease is common. One in 10 people in Canada suffers from it.
The slide showed that the surgical mortality of kidney donation was three deaths per 10,000, which is a little riskier than a vaginal delivery (one death per 10,000) but less than a C-section (up to 10 deaths per 10,000) and significantly less than a liposuction (up to 20 deaths per 10,000). Of course, complications can always happen but for the most part they were minor, like a urinary tract infection or pneumonia.
When I talked about it with others, one question came up. What if I needed a kidney one day? Or if someone I love did? The risk is low, but the medical team reassured me I would be at the top of the waitlist. There is even a national program under development for donors to identify people around them who could eventually require a transplant. If one of them ended up needing a new organ, they would be on a priority list.
I also discovered an American online support group, Kidney Donor Athletes, and met a transplant twin with the same surgery date as me. We exchanged some encouraging words and pictures of our IV lines.
A brief history of organ donation
Until the 1950s, kidney failure was a death sentence. Dialysis had just been discovered, and the idea of transplanting a kidney from one person to another was a futuristic pipe dream. By the late 1960s, many organs had been transplanted. But it was only in 1983, with the approval of cyclosporine, a drug that inhibits immune system activity and thus prevents organ rejection, that transplants took off.
In December 1954, Richard Herrick was the first recipient of a donated kidney. Aged 23, he suffered from severe kidney disease and his days were numbered. His brother, Ronald, was ready to do anything to save him. He told doctors he’d give Richard one of his own kidneys if he could. It had never been done. The doctors thought the transplant couldn’t possibly work, that Richard’s body would reject the new organ. Unless…Richard and Ronald were identical twins. Would that make a difference?
The two brothers were referred to Dr. Joseph E. Murray of Harvard, who would be awarded the Nobel Prize in medicine in 1990 for his work on transplants. Murray had started his career as a plastic surgeon in the 1940s, using skin grafts to rebuild the hands and faces of Second World War survivors. After the war, he joined a group of researchers interested in kidney failure.
When the Herrick brothers came to him, he was at first reluctant. Did Ronald really understand the implications of his donation? Early data seemed to show that living with a single kidney was not particularly risky, though evidence was scarce. In addition, there was the risk of surgery itself, which was hard to assess. Murray and his team consulted many colleagues, lawyers and even priests before securing permission from the family.
The night before surgery, Richard sent an urgent missive to his brother’s room: “Get out of here and go home!” Ronald was steadfast: “I am here, and I am going to stay.”
The surgery was successful. Ronald’s kidney was grafted in Richard’s lower iliac fossa (lower abdomen), as it is done today. Recovery was swift. Richard left the hospital after two weeks, having taken advantage of his stay to court the nurse who cared for him. They got married and had two children. The transplant allowed Richard to live another eight years, until the disease attacked his new kidney, Murray wrote in Scientific American. Ronald lived to be 79 years old.
Transplant between twins continued into the early 1960s. Immunosuppressive drugs later made it possible to transplant organs from deceased donors and non-twin living donors. In 1962, Murray successfully transplanted a kidney from a non-related donor. Despite those advances, medical professionals long believed that donations from blood relatives were preferable.
Admittedly, nephrectomy (the surgical removal of a kidney) used to be more painful and invasive than it is today. Until the 1990s, it was necessary to break one of the donor’s ribs, leaving a substantial scar. Today, laparoscopic surgery allows doctors to insert instruments and cameras through only four little openings in the abdomen, in addition to a short incision above the pubic bone, similar to a C-section.
Though organ donations now make it theoretically possible to offer a nearly normal quality of life to people with kidney failure, a problem remains: too few kidneys are available.
Altruism
I was surprised to discover that in North America, until the early 2000s, donating an organ to a stranger — as I did — was prohibited. According to a 1971 article in Seminars in Psychiatry, physicians considered non-directed kidney donation to be “impulsive, suspect and repugnant.” The medical profession could not consider the surgery justifiable unless the donor genuinely benefited from it, such as a mother wanting to save her daughter from endless dialysis, sparing herself the sadness of seeing her kin suffer or die. Without personal interest, the gesture seemed to have no meaning.
The first documented non-directed kidney donation from a stranger is that of Sunyana Graef in 1999. Her surgeon told her story in the journal Nephrology Dialysis Transplantation. Graef was the founder of the Vermont Zen Center and communicated with a Massachusetts hospital to donate a kidney, having never heard of anonymous organ donation before. To her, donating was an extension of her Buddhist calling to help all beings. But the hospital declined her offer.
Graef then contacted Brown University’s kidney transplant program and shared her wish to donate. No, she was not “crazy.” Yes, generosity was a legitimate reason to proceed. The transplant team accepted the reasoning.
Today, most North American transplant centres accept non-directed donations. These anonymous donations are few in number but increasing every year. In the United States, there were 405 in 2021, up from only five in 2000. Although data is hard to come by, a growing number of people on kidney transplant waitlists also find donors through social media or on specialized internet forums.
Thankfully, in Canada, patients’ autonomy is honoured and non-directed organ donations are integrated with transplant centres’ living donation programs. Donors do not need to be protected from themselves. Nevertheless, there are only about 30 every year in Canada, including a handful in Quebec. My decision, though welcome, was surprising for my caregivers.
Early in the process, the nephrologist asked me an unexpected question: did I prefer to donate to someone on the Transplant Québec list or through the Kidney Paired Donation (KPD) program operated by Canadian Blood Services? I hate making decisions. As a vegan, I am used to not having many choices at restaurants and I like that. I let my hairstylist do what she wants with my hair. I trust Netflix to recommend new shows to me. But this was up to me.
Transplant Québec manages the list of every person awaiting an organ transplant in the province. The list currently has 620 names. As soon as a kidney becomes available, either because someone dies or when an anonymous donor presents themselves, the organ is allocated based on various criteria, including how long the patient has been on dialysis, whether the tissues are compatible, and the antibody rate (patients with more antibodies have a harder time finding an organ and get priority). Every province has its own similar agency and process.
Meanwhile, since 2009, Canadian Blood Services has been administering its KPD program across the country. The program is based on the fact that some people who are hoping for a kidney donation are biologically incompatible with those who wish to donate one to them. Let’s say that your friend needs a kidney, and you would love to help, but compatibility tests show that her body would reject your kidney. Thanks to the KPD program, you could be matched with another duo in the same situation. In the simplest scenario, the donor from pair A would donate a kidney to the receiver of pair B, and vice versa.

In a more common scenario, managed by Canadian Blood Services and comprising around 60 percent of cases, a domino chain is set up. A donor without a pre-designated receiver gives their kidney to the receiver of pair A (let’s say that’s your friend). You then donate your kidney to the receiver of pair B, the pair B donor gives a kidney to the receiver of pair C, and so on. The last kidney of the chain is donated to a compatible receiver on the waitlist of the original donor’s province. If I donated through the KPD program, a kidney would still end up being donated to someone on the Transplant Québec list.
The right choice became obvious. Through KPD, my kidney gained super-powers and would go on living somewhere else in the country, becoming part of a chain of solidarity.
As Dr. Joshua D. Mezrich wrote in his 2019 memoir, When Death Becomes Life: Notes from a Transplant Surgeon: “The sick suffer alone, they undergo procedures and surgeries alone, and in the end they die alone. Transplant is different. Transplant is all about having someone else join you in your illness.”
Overcoming shortage
Celebrities like Tina Turner, Stevie Wonder and Selena Gomez owe their lives to kidney donations. But most people who live with kidney failure have not been so lucky. In 2021, in Canada alone, 103 people died before receiving the transplant that would have saved their life. Currently, approximately 3,000 Canadians are hoping for a new kidney, while 1,619 surgeries were performed last year.
Meanwhile, news sources talk about organ shortage as they talk about climate change: it’s a complex, depressing issue that we don’t understand very well and that few people get excited about. Of course, we are reminded that we can sign our organ donor card and make sure our loved ones know our wishes.
In reality, the odds of our organs being donated when we die are slim. In 2012, of the 156,464 people who died in a Canadian hospital, only 3,088 were identified by the Canadian Institute for Health Information as organ donor candidates (they had explicitly consented to donating and their organs were not substantially damaged). Many factors further constrain donations from deceased donors, such as poor identification of organs by medical staff, too few transplant teams, insufficient hospital resources and family disagreements. Of the potential candidates, only 520 ended up donating.
At the end of 2021, for the first time, a kidney from a genetically modified pig was grafted onto a human. A second case, from the University of Alabama at Birmingham, was reported a few weeks later in the American Journal of Transplantation.
The idea of animal-to-human organ transplants can be shocking. Whether they are feasible and constitute a long-term solution remains unknown. The grafts were done on brain-dead patients and were only monitored for a few days. Yes, the grafted kidneys were able to create urine. But kidneys are complex. Can a pig kidney play the same roles as those required in the human body? Who will get the donated organs? What is the cost?
One may also wonder whether the news of the first cross-species transplant was foremost a scientific or marketing feat. The pigs were provided by Revivicor, a spin-off of PPL Therapeutics. The latter made headlines in 1996 after creating the first mammal clone in history, Dolly the sheep. Revivicor is now a subsidiary of United Therapeutics Corporation, a biotechnology company that bankrolled the transplants. At press time, UTC’s stocks were trading at $226, after gaining more than 25 percent in the past year.
Those attempts at xenotransplants remind us that humans have long been exploiting those they consider inferior for their kidneys, livers, hearts, lungs and eyes. In India, for instance, women account for only 22 percent of organ receivers but represent 74 percent of live donors. Women are expected to donate organs but are less likely to be considered worthy of receiving one. There are stories of men who married a woman solely to receive a kidney from her.
In the Squid Game Netflix series, millions were horrified to see deceased losers’ organs harvested for sale. Unfortunately, that is not entirely fictitious. Last year, an independent expert group of the United Nations shared its concerns about allegations of organ harvesting among jailed individuals from Chinese minorities, notably Falun Gong followers, Uyghurs, Tibetans and Christians. The Chinese situation is not unique. The World Health Organization estimates that 10 percent of organs transplanted around the world come from the black market.
According to the International Registry on Organ Donation and Transplantation, Canada had 10 living donors per million in 2020, whereas countries like New Zealand and Israel had rates of 18 and 35 living donors per million respectively. How come?
In New Zealand, donors are fully covered against financial loss for up to 12 weeks after surgery, while in Quebec the maximum reimbursement is only $5,715. I am privileged. I live near the hospital, and I have disability insurance. My insurer agreed to pay for my sick leave! But most people cannot afford to take several weeks off work.
In Israel, almost 70 percent of donations are owed to living donors, a unique situation that’s largely attributable to a single organization, Matnat Chaim (translated as the “Gift of Life” or “Living Gift”). The group recruits donors in the Orthodox Jewish community, creating a virtuous circle. An article in BMC Nephrology attributed Matnat Chaim’s success to its religious roots. A passage of the Talmud reads, “Whoever saves one life saves the world entire.” However, I believe that some aspects of the program can be imitated in the secular world: sharing stories about dialysis, information sessions on donation, and donors who can share their experiences.
Through all this, I feel like I have added meaning to my life. I feel like I have been part of something greater than myself. I was able to help, for real.
In hindsight, I realize that a lot needs to be done to promote living organ donation in Canada. Had I not heard my colleague’s story, I would never have known it was even possible. Currently, the majority of living donors make directed donations, and those suffering from kidney failure are encouraged to look for a donor in their own circles. Internet forums are filled with heart-wrenching messages. These would-be recipients need better options. Living donor kidneys should not be reserved for those with a tear-inducing story or a broad network on social media.
In 2013, 49 percent of Americans said in a survey that they would be “very” or “somewhat” likely to consider donating a kidney to someone they had never met. As far as I know, a national survey like this hasn’t been done in Canada, but I see no reason why we would be less altruistic than our southern neighbours.
It has been almost a year since I donated my left kidney. The day after surgery, I was walking through the hospital, pulling my IV along, to enjoy the view of the sunrise over Jacques Cartier Bridge. Two days later, I was home, and I quickly felt better. Pain was never unmanageable, and Tylenols were great. My most recent blood tests show that my right kidney works perfectly and my scars have healed.
Through all this, I feel like I have added meaning to my life. My day-to-day is the same, but I’ve gained perspective that allows me to see the world differently. My life is no longer limited to planning my next trip, sitting in Zoom meetings or ordering organic wine from the liquor store. I feel like I have been part of something greater than myself. I was able to help, for real.
When I talk about that kidney of mine that now filters someone else’s blood, I’m often asked how I found the courage to donate. I don’t know for sure, but I don’t see myself as courageous. I just feel that it was the right thing to do.
***
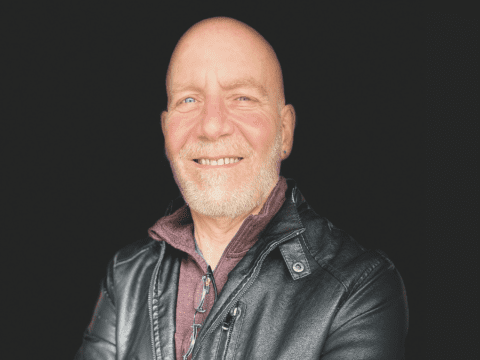
Élise Desaulniers is a writer and former executive director of the Montreal SPCA.
A version of this article originally appeared in the French magazine Nouveau Projet in April 2022. It also appeared in Broadview’s October/November 2022 issue with the title “Gift of a lifetime.”