Throughout the four years that Suzanne Smith worked as a housing co-ordinator for a social service agency in Hamilton, she loved her job.
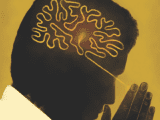
Her clients were people who struggled with mental illness. Locating supportive housing for them was often a challenge, but Smith found it highly rewarding. So, she was devastated when she was suddenly hit with debilitating fatigue, headaches and muscle pain, as well as depression and anxiety, making it impossible for her to do her job.
You may unsubscribe from any of our newsletters at any time.
It took several months and several tests before she was diagnosed with myalgic encephalomyelitis, a chronic neuro-immune disease that causes physical and mental health problems. The agency’s executive director was supportive and urged her to take the time off she needed.
“She knew my work record and said, ‘We have enough faith in you that we’ll pay your benefits while you’re off,’” says Smith, who asked that her real last name not be used.
Four months later, her doctor approved her return to work. When Smith contacted the agency, she learned that a new director had been hired. “I went and met with [the new director], thinking I was coming back to work, and she said, ‘I had a friend who had what you have, and she can’t do her job. So it’s my opinion that you can’t work, so we’re going to let you go.’ I was absolutely gobsmacked and just sat there. I was in shock.”
Smith tried to show the director her doctor’s note and argue that she was incorrect. “She just kept doodling on a notepad and didn’t even look at me,” says Smith, who was 35 at the time.
The meeting lasted less than five minutes. If the agency had a workplace policy around mental health leaves, Smith wasn’t aware of it and didn’t have the finances to hire a lawyer. She had no choice but to walk away. “The circuitous irony is that this was an organization that supported people with mental health issues, and it was being run by someone who didn’t understand the concept of mental health issues and was making bad decisions toward people who had mental health problems,” says Smith.
Although her situation occurred 22 years ago, Smith’s story is not uncommon today. Despite the fact that mental health problems extract huge costs from both employees and employers, only 42 percent of Canadian organizations have a workplace mental health policy in place, according to a 2016 Conference Board of Canada report.
On any given week in Canada, more than 500,000 people will miss work due to a mental health problem. That amounts to huge personal losses, as well as sky-high economic costs. In Canada, workplace mental health is estimated to cost the economy around $50 billion a year, according to the Mental Health Commission of Canada.
Globally, employees with untreated depression lose about 11 days of work a year (on average) as a result of their mental health problems. Depression and anxiety are the two main workplace mental health illnesses. Indeed, the World Health Organization has declared depression the top cause of disability in the world today.
In workplaces, there’s also the issue of “presenteeism” — when an employee comes to work but cannot do his or her job well due to mental health concerns. Because mental illness can bring on sleep problems, sluggishness and overwhelming emotions of sadness and anger, a person may have difficulty being fully productive.
A 2015 survey by Morneau Shepell, an international human resources consulting company, revealed that 82 percent of employees with mental health issues said that their condition impacts their work, compared to 53 percent of those with physical health issues.
With so much at stake, why are employers lagging behind in developing workplace mental health policies? Like so many issues involving mental illness, it all starts with stigma.
Many employees fear they’ll pay a heavy price if they disclose their mental health problem, either by being shut out of projects or losing their job, says Dave Gallson, associate national executive director of the Mood Disorders Society of Canada. It’s a well-founded fear, according to a 2011 Conference Board of Canada report. Among employees who did reveal a mental health issue, 27 percent said it negatively affected their careers.
“So many workplaces think if they open up about mental illness at work it will cause more problems, but it’s already costing them far more by not addressing it,” says Gallson. The first step toward creating a workplace mental health policy, he adds, is to create an environment where it’s safe for employees to talk about their mental health struggles. That means changing the culture to let people know they can step forward and talk.
“What we’ve found with many employers is that once you create an avenue to allow employees to talk openly, then they will really lead the charge and progress within the organization and develop and implement the tools needed to bring issues to light,” he says.
Managers, too, can be reluctant to broach the issue because they believe they’re not well versed in mental health issues and fear overstepping their boundaries or saying something wrong. But as Gallson says, “Managers don’t need to be psychologists. They just need to be good listeners and be aware of resources in the community.”
The Mood Disorders Society of Canada developed an anti-stigma campaign called “Elephant in the Room,” which includes posters, brochures and small blue elephants, all designed to assist organizations in raising awareness. Gallson says some managers perch a blue elephant on their desk to demonstrate to employees that their office is a safe place to talk about mental illness.
The campaign has been used by police departments, schools and universities, and in countries like Ireland and the United Kingdom. The society also produced Workplace Mental Health, a booklet that promotes wellness and offers step-by-step ideas on setting up a plan. Given that it’s been downloaded about 22,000 times, Gallson believes there’s a growing interest among employers to develop strategies.
But what if the workplace environment itself is causing the stress? It’s a valid question given the findings of the Morneau Shepell survey, which showed that a stressful workplace can affect the mental well-being and productivity of employees. “Currently we are in an environment where increasing demands and an increasing rate of workplace change is the norm,” Paula Allen, a vice-president at Morneau Shepell, writes in an email. She believes that if an organization wants to maintain a productive workforce, it needs to invest in mental health.
Louise Chénier, program manager of workplace mental health at the Mental Health Commission of Canada, helps employers create a mentally healthy work environment and says that it makes sound financial sense to do so. In Canada, 30 percent of both short- and long-term disability claims are for mental health issues; however, they represent 70 percent of medical costs because people tend to take more time off for mental health issues, often due to wait times for treatment, says Chénier.
Employers who fail to implement such policies are also at risk of being caught in legal issues related to psychological injury and could be challenged under employment contract law or the human rights code. “Just like you’d have a safety standard for those who work in an enclosed environment or those who are working [at] heights, you need one for mental health,” Chénier says.
Four years ago, the Mental Health Commission released an initiative, the National Standard of Canada for Psychological Health and Safety in the Workplace, to help employers improve their approach to promoting mental health. It encourages employers to identify workplace hazards, such as stressors from job demands.
Michael Garron Hospital in east Toronto was one of 40 companies included as a case study in the initiative. In three years, it saw a seven percent decrease in health-care costs related to mental health, as well as a decrease in the absenteeism rate from 10.6 to 6.5 days a year. Chénier says the hospital achieved that by identifying risk factors in the workplace and putting programs in place.
One in five Canadians will experience a mental health issue in the next year, which means that 20 percent of the workforce could be affected. For many people, the biggest challenge in taking a mental health leave is the fear of being perceived differently upon their return.
That’s something Scott Gardner thought about when he was off work for four months with depression. Gardner’s photos have graced many front pages at the Hamilton Spectator, the newspaper where he works. Seven years ago, his father died, setting off his slow spiral into depression. He hadn’t begun to deal with the loss when he suffered a concussion while playing hockey.
Over the next several months, he felt increasingly anxious. “It felt like my brain was vibrating,” Gardner says. One afternoon, the fast-paced energy of the newsroom, something he usually enjoys, was suddenly too much to handle.
“I remember I was sitting at my desk, and I remember thinking I had to go. It was like a screw came undone, and I thought, I’m done. I just walked out,” says Gardner, who is 52. “I spent a lot of time that week under the covers just trying to shut out the noises. There were times when it wouldn’t shut up. I was shaking, and I felt confused and panicky, like I wanted to turn my brain off but couldn’t.”
His symptoms worsened. A panic attack in a grocery store was so severe that he had to call his wife to come get him. His doctor diagnosed him with clinical depression and prescribed an antidepressant. He credits his social worker for helping him recognize the behaviour patterns that were leading him into a depressive episode. “I just needed to realize what a machine the brain is and that really all these moods are because of that.”
Four months later, Gardner returned to work on gradual re-entry, starting with half days and shorter workweeks. His supervisor accommodated his request to move out of management and into a less stressful job. He credits the support he received from his managers with helping him to ease back into work, and adds that his return had a somewhat amusing side.
“At the first meeting when I got back, everyone was so nice to me. They were giving me all kinds of compliments. It was kind of funny, but it was kind of nice too. I think they were thinking, ‘Is he going to snap again?’ I noticed people gave me a wide berth when they saw me coming.”
The experience permanently altered his perspective on life. “If I’m feeling crappy, my job doesn’t come first anymore, not at the expense of my health,” Gardner says. “I still do my job, and I do my best at it. I try to be the best I can, but if I’m feeling really nauseous, I cut back.”
It’s an attitude many in the mental health profession think is long overdue. Says Gallson, “Employers should understand that to have their worker back and to create a healthy workplace where they can do their job . . . is to everyone’s benefit.”
This story originally appeared in the May 2017 issue of The Observer with the title “Calling in Sad.”